The Australian Government is now in caretaker period. During this time, updates on this website will be published in accordance with the Guidance on Caretaker Conventions, until after the election.
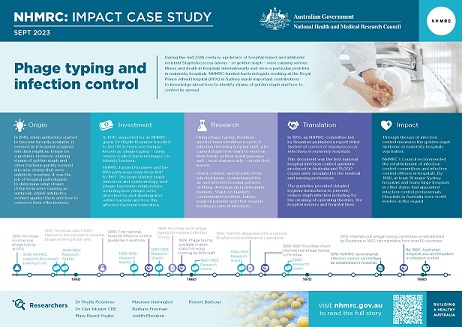
During the mid-20th century, epidemics of hospital-based and antibiotic resistant Staphylococcus aureus – or golden staph – were causing serious illness and death in hospitals internationally, and one strain was a particular problem in maternity hospitals. NHMRC-funded bacteriologists working at the Royal Prince Alfred Hospital (RPA) in Sydney made important contributions to knowledge about how to identify strains of golden staph and how to control its spread.
Origin
In 1945, when antibiotics started to become broadly available, it seemed as if hospital-acquired infection and infection control might no longer be a problem. However, existing strains of golden staph and other bacteria quickly evolved into, or were replaced by, new strains that were antibiotic resistant.
In newborn babies, golden staph infection can colonise mucous membranes or skin without causing symptoms. It can cause mild symptoms such as ‘sticky eye’, various types of sores and lesions, and infections around the finger and toenails and the umbilical cord stump. More seriously, it can cause problems such as pneumonia, osteomyelitis (inflammation or swelling of the bone) and septic arthritis (an infection in joint fluid or tissues). In surgical patients, a serious golden staph infection can cause septicemia (sepsis, or blood poisoning) which in turn can lead to septic shock and death.
Hospital pathologists determine what strains of bacteria are causing an outbreak, which antibiotics will work against them, how to conserve the effectiveness of those antibiotics and how to minimise the spread of bacteria within the hospital. In 1938, when bacteriologist Dr Phyllis Rountree commenced work at the Fairfax Institute of Pathology – RPA’s pathology laboratory – she was already very familiar with golden staph. She was also familiar with the viruses that prey on them, known as bacteriophages (phages), which she had studied while working with future Nobel laureate Frank Macfarlane Burnet at the Walter and Eliza Hall Institute in Melbourne.
Credit: iStock, iLexx
Bacteriophages attacking a bacterium
Investment
In 1947, and supported by an NHMRC grant, Rountree joined the Staphylococcal Reference Laboratory of the British Ministry of Health, learning a technique known as ‘phage typing’ – using bacteriophages to identify bacteria.
During the period 1947 to 1967, Rountree and the RPA pathology team, which (over time) included Mary Beard, Maureen Harrington, Barbara Freeman, Judith Rheuben and Robert Barbour, were continuously funded by NHMRC to study staph infections and epidemiology, and phage-bacterium relationships.
The PDF poster version of this case study includes a graphical timeline showing NHMRC grants provided and other events described in the case study.
Credit: Claas Kirchhelle 1
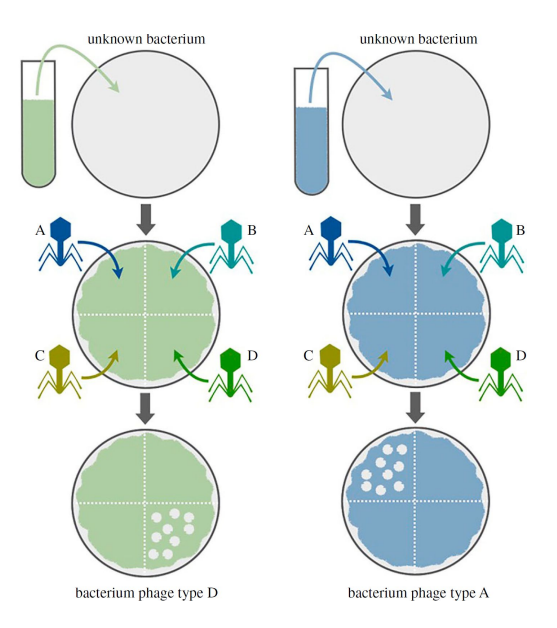
Phage typing involves creating a ‘lawn’ of an unknown strain of a particular bacterial species (such as S. aureus) then introducing known types of phages to different areas of the lawn, to see which combination of phages the bacteria are vulnerable to.
Research
Phage typing
In 1945, and as part of RPA’s routine pathology work, Rountree began phage typing bacteria collected in RPA’s surgical wards.2 Beginning in 1952, her team’s work began to take on national significance when hospitals around Australia began experiencing outbreaks of neonatal (newborn baby) infection. This was due to a new phage type of S. aureus, which they designated as ‘type 80/81’.2,3,4
By 1955, type 80/81 was responsible for most outbreaks of neonatal infection across Australia and had also been isolated from such epidemics in New Zealand, Canada, France and the UK. By 1957, the RPA team was typing cultures not only from its own hospital inpatients but also from samples sent by other hospitals in the Sydney area, 20 other NSW localities and other states.
In 1958, Rountree led the phage typing component of a National Survey of Soft Tissue Infections in General Practice. This survey, organised and funded by the Australian Government Department of Health at the recommendation of NHMRC, found a widespread prevalence of type 80/81 outside of hospitals, and that 91% of samples of type 80/81 were penicillin resistant. This led to the conclusion that penicillin could no longer be used against serious staph infections unless the sensitivity of the strain was already known. The results of this survey were published in 1960 as an NHMRC Special Report.5,6
Antibiotic resistance
The bacterial cultures obtained by the RPA team were routinely tested for antibiotic resistance. Over the period 1949 to 1962, the proportion of cultures that were penicillin resistant increased almost continuously, as did the number of strains resistant to more than one antibiotic. These statistics were reported annually to NHMRC (refer Table 1).
There was one type of antibiotic that many staph strains were still sensitive to: erythromycin. First isolated in 1952, it started to become available in Australia in 1953. At that time, NHMRC’s Council recommended that use of erythromycin be confined to treatment in hospitals. At RPA, use was further restricted to infections resistant to all other antibiotics.
| Year | No. cultures examined total/outpatients* | % resistant to penicillin | % resistant to antibiotics (#) |
|---|---|---|---|
| 1949 | 228 | 53 | 5.9 (2) |
| 1950 | 491 | 53.7 | 23.8 (2) |
| 1951 | Not reported (NR) | 62 | 9.5 (4) |
| 1952 | 1,332/455 | 67.8 | 19.4 (4) |
| 1953 | 2,020/182 | 70.6 | 2.8 (5) |
| 1954 | 2,400/327 | 62.7 | 5 (5) |
| 1955 | 3,900/680 | NR | NR |
| 1956 | 3,630 | 76.7 | NR |
| 1957 | 3,580 | 75.2 | 6 (all available) |
| 1962 | NR | 80 | NR |
| 1963 | NR | 65 | NR |
* This column shows the total number of cultures examined (i.e. from both inpatients and outpatients) followed by the number of cultures examined only from outpatients. So, in 1955, 3,900 cultures were examined in total, and of these, 680 came from outpatients.
# The number in brackets is the number of antibiotics other than penicillin to which cultures were resistant.
Infection control
Using phage typing, Rountree and her team identified cycles of infection involving hospital staff, who carried staph from ward to ward on their hands, in their nasal passages and – most dangerously – on infected lesions. Direct contact and droplets from noses, colonised by S. aureas, contaminated the air, hospital surfaces, clothing, dressings and particularly blankets. Staph on blankets contaminated mothers, babies, surgical patients and their wounds, leading to clinical infections. Patients in turn contaminated the blankets which, during bedmaking, spread staph contaminated dust particles into the air, starting the cycle again.
Credit: iStock: dusanpetkovic
Hand hygiene is a basic feature of hospital infection control
The team studied contamination by type of blanket (wool, cotton) and found that infection control was mainly about frequency of washing. The team also found that bathing of babies with an antibacterial lotion caused a large drop in the infection rate. Fundamentally, they found that the most dangerous source of infection was a clinically infected or colonised staff member moving about the hospital and interacting with patients. They identified that the aim of infection control must be to eliminate all sources of infection and to reduce contact spread at all times.
By 1962, the use of nasal antibiotics had been adopted for all patients admitted to the RPA surgical unit. This resulted in a significant reduction in nasal carrier rates and associated wound sepsis. However, because the presence of one type of staph impeded the establishment of other strains, and because strains differed in their level of antibiotic resistance, the team found that the long-term use of antibiotic nasal creams would encourage antibiotic resistant strains to thrive at the expense of other strains. In fact, some strains would only grow in the presence of an antibiotic.
In 1963, with the introduction at RPA of single rooms and ventilated cubicles for patients, staph contamination dropped significantly, and the nasal carrier and wound infection rates also dropped.
The seriousness of antibiotic-resistant infection was demonstrated when the team studied the incidence and mortality rate of generalised staph infection at RPA over the period 1950-1957. Of patients admitted with serious infection, the mortality rate was 50%. Of those acquiring serious infection in hospital, the mortality rate was 86%. However, during 1963 there was no case of staph septicaemia acquired in the hospital. Reasons for the fall were thought to include the refurbishment and cleaning of the wards, use of new synthetic penicillins and the use of nasal antibiotics.
Phage studies
Rountree studied a wide range of features of phages and their relationship with bacteria, including how phages were absorbed and disintegrated within bacteria and how this affected bacterial replication. In 1952, Rountree visited CSIRO’s Division of Industrial Chemistry to use electron microscopy to better understand what happens when phages enter staph cells.
Rountree also studied environmental factors that played a role in the phage-bacteria relationship. For example, she found that calcium ions were essential for phage replication and synthesis. In the absence of calcium, the staph cells were immune to attack by phage. She also examined the effects of ultraviolet light on phages and bacteria.
Her studies of phage genetics found that strains of type 80/81 staph could be converted to other strains if a bacteriophage’s DNA was incorporated within the bacterial DNA. She also studied the genetics of staph antibiotic resistance and found that genes controlling resistance to antibiotics could be located either on the bacterial chromosome, or outside of it on a special entity situated in the bacterial cell, known as an episome.
Translation
International Committees
In 1952, the results of three and a half years of phage typing by the RPA laboratory were compared with results from the UK’s Staphylococcal Reference Laboratory. This was the first large-scale ecological survey of the distribution of different types of disease-causing staph in human beings.
In 1953, Rountree co-established the International Association of Microbiological Societies Sub-Committee for Phage Typing of Staphylococci. She served as chair from 1966 to 1982.7 By 1978, the sub-committee included membership from over 50 countries.2
By 1956, Rountree had established a Staphylococcus Reference Laboratory at RPA, which NHMRC designated as a national reference laboratory in 1965.
NHMRC Committees
In 1954, in response to the hospital nursery staph epidemic, NHMRC’s Council established a five person committee – whose membership included Rountree and paediatrician Dr Clair Isbister – to ‘inquire into the present and possible future extent of the problem, its treatment and prevention’.
Published in 1956, the Committee’s final report – drafted by Rountree and Isbister – was titled System of control of staphylococcal infections in maternity hospitals. This document was the first national hospital infection control guideline produced in Australia and 15,000 copies were circulated to the medical and nursing professions. The document included detailed hygiene instructions for operating theatres, dressing trolleys, umbilical cord dressing, feeding and nappy changing, bathing equipment and cleansing the baby, blankets, cot linen and the hospital nursery.
Rountree was a member of NHMRC’s Antibiotics Committee from 1963 to 1969. In 1964, and following practice established at RPA a decade earlier, the Committee recommended erythromycin should be restricted to the treatment of serious infection not able to be treated by other antibiotics.
Outcomes and impacts
Infection control
The type 80/81 epidemic in Australian maternity hospitals continued until the mid-1960s when it was halted by the almost universal adoption of washing babies in an antibacterial soap containing hexachlorophene.2
The 1958 survey of staph infection in general practice was the first of its kind in the world.8 In 1959, following the survey, some Australian states began a Staphylococcal Service designed to undertake prompt antibiotic sensitivity testing of cultures of staph supplied by medical practitioners.
In 1976, NHMRC’s Council noted that hospital-acquired infections and their associated morbidity, mortality, and economic consequences were a significant problem in Australia and that the extent of the problem was not always appreciated by hospital administrations. Council recommended that state and territory health authorities consider the establishment of infection control committees and infection control officers in hospitals. By 1980, at least 14 major Sydney hospitals and many large hospitals in other states had appointed infection control professionals. Hospitals in Australia and the UK were world leaders in this regard.
Hospital infection prevention and control remains of vital concern to health care. A recent World Health Organisation report shows that, where good hand hygiene and other cost-effective practices are followed, reductions of health care-associated infection rates in the range of 35%–70% are possible, irrespective of a country’s income level.9
Phage typing
Rountree’s use of phage typing in infection control at RPA led efforts in Australia. By 1959, phage typing services had become available in each state with the service providers having been trained at RPA.
The use of bacteriophages to type bacteria was an important tool of twentieth-century epidemiology.1 Rountree was a prominent figure within the global phage typing community from the 1950s onwards and her team played a key role in uncovering the global spread of the first pandemic of antibiotic resistant type 80/81 staph.
Phage therapy
Rountree’s investigations of the phage-bacterium relationship opened lines of investigation that are now being pursued by NHMRC-funded researchers into the use of phages as antibacterial therapy.10
Researchers
Dr Phyllis Rountree
Phyllis Margaret Rountree (1911-1994) completed Bachelor and Master of Science degrees at The University of Melbourne then undertook a Council for Scientific and Industrial Research (CSIR) fellowship at the Waite Agricultural Research Institute (1931-1934). Rountree was then employed as a researcher at the Walter and Eliza Hall Institute (1934-1935), studied for a post-graduate Diploma in Bacteriology at the London School of Hygiene and Tropical Medicine and worked at the Public Health Laboratory in London (1936-1937). She was a Clinical Bacteriologist in the Bacteriology Laboratory at St Vincent's Hospital, Melbourne (1938-1943) then a Research Bacteriologist at RPA (1944-1961).
Rountree completed a Doctor of Science (DSc) at The University of Melbourne in 1950. She was Chief Bacteriologist at RPA (1961-1971) and then a Consultant Bacteriologist (1971-1992). She was made an Honorary Life Member of the Australian Society for Microbiology and was awarded an honorary Doctor of Science degree from The University of Sydney in 1987. In 2021, the newly established bacteriophage family Rountreeviridae was named in Rountree’s honour.
Dr Clair Isbister CBE
Jean Sinclair (Clair) Isbister (1915-2008) won scholarships to study at The University of Sydney, where, in 1938, she received a Bachelor of Medicine. In 1949, she received a Diploma of Child Health from the University of London. Isbister worked at RPA and then at the Royal Alexandra Hospital for Children (now The Children’s Hospital at Westmead in Sydney). In 1948, Isbister became a consultant paediatrician at Royal North Shore Hospital, a position she held until her retirement in 1980. Isbister was created an Officer of the Order of the British Empire in 1969 and a Commander of the Order in 1977, for her services to medicine.
Mary Beard-Pegler
Mary (Molly) A Beard-Pegler was a Senior Research Officer and member of the RPA pathology team for over 45 years. After Phyllis Rountree’s retirement, Beard-Pegler went on to work extensively with Alison Vickery, who took over Rountree’s phage typing responsibilities at the Fairfax Institute. Between 1958 and 2003, Beard-Pegler was co-author on at least 23 publications related to hospital infection control and microbiology, particularly with respect to antibiotic resistant staph.
Partner
This case study was prepared with input from Professor Lyn Gilbert AO and Professor Jonathan Iredell and in partnership with The University of Sydney.

References
The information and images from which impact case studies are produced may be obtained from a number of sources including our case study partner, NHMRC’s internal records and publicly available materials. Key sources of information consulted for this case study include:
-
Kirchhelle C. The forgotten typers: The rise and fall of Weimar bacteriophage-typing (1921–1935). Notes and Records. 2020 Dec 20;74(4):539-65
-
Rountree PM. History of Staphylococcal infection in Australia. The Medical Journal of Australia 1978. 2:543-546
-
Hillier K. Babies and bacteria: phage typing, bacteriologists, and the birth of infection control. Bulletin of the History of Medicine. 2006 Dec 1:733-61.
-
Rountree PM and Freeman BM. Infections Caused by a Particular Phage Type of Staphylococcus Aureus. Medical Journal of Australia 1955, 2:157
-
A Survey of Staphylococcal Infections of the Skin and Subcutaneous Tissues in General Practice in Australia. The British Journal of General Practice 1960 Nov;3(4):498–500
-
Johnson A, Rountree PM, Smith K, Stanley NF and Anderson K. A. Survey of Staphylococcal Infections of the Skin and Subcutaneous Tissues in General Practice in Australia, May-December, 1958. NHMRC Special Report Series No. 10. Canberra, 1960
-
Obtained from https://labouraustralia.anu.edu.au/biography/rountree-phyllis-margaret-27706. Accessed 17 May 2023
-
Editorial. Staphylococci at large. The Journal of the College of General Practitioners 1960; 3(4): 396
-
Global report on infection prevention and control. Geneva: World Health Organization; 2022.
-
Schooley RT and Strathdee S. Treat phage like living antibiotics. Nature microbiology. 2020 Mar; 5(3):391-2.