The Australian Government is now in caretaker period. During this time, updates on this website will be published in accordance with the Guidance on Caretaker Conventions, until after the election.
Road Map 3: A strategic framework for improving Aboriginal and Torres Strait Islander health through research. Report of Community Consultations.
Linked to:
Publication Data
Executive summary
The National Health and Medical Research Council (NHMRC) has committed to develop Road Map 3: A strategic framework for improving Aboriginal and Torres Strait Islander health through research (Road Map 3) to guide and communicate its objectives and investment in Aboriginal and Torres Strait Islander health research for the next decade. Road Map 3 follows on from the release of Road Map 1 in 2002 and Road Map 2 in 2010.
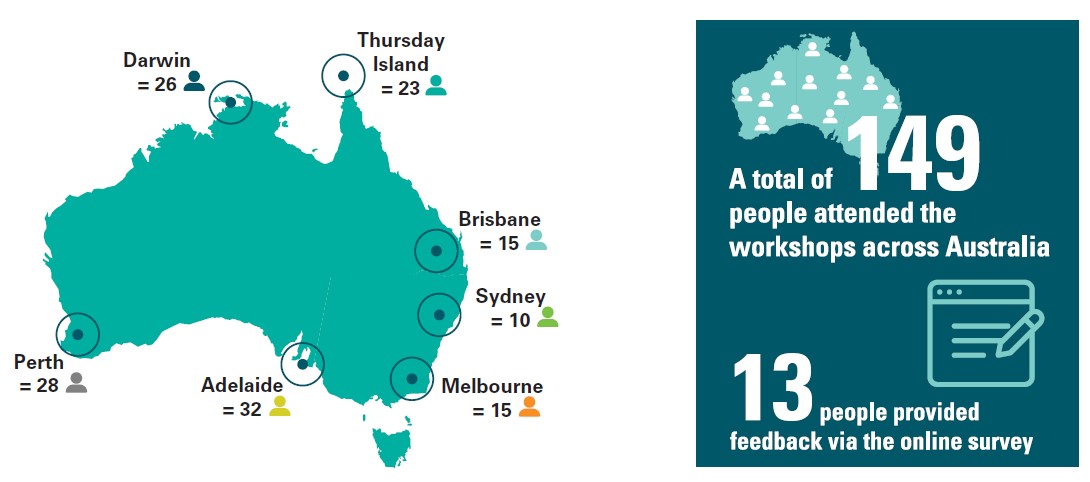
- Image description - Figure 1
Infographics showing the location of workshops and number of participants.
- A total of 149 people attended the workshops across Australia.
- 13 people provided feedback via the online survey
- Darwin = 26
- Thursday Island = 23
- Brisbane = 15
- Sydney = 10
- Melbourne = 15
- Adelaide = 32
- Perth = 28
From March to July 2017, NHMRC and its Principal Committee Indigenous Caucus (PCIC)1 worked with Nous Group (Nous) to conduct a national consultation process for the development of Road Map 3. This report provides a summary of the outcomes of these consultations, preliminary workshops, and will form a reference in Road Map 3 when it is released for public consultation and thereafter, publication.
The consultation process for Road Map 3 began in March 2017 and involved interviews with nine leaders of Aboriginal and Torres Strait Islander health and research peak bodies and seven workshops across Australia (see Figure 1 above) attended by researchers, health workers, government officials and community leaders. For those who could not attend the workshops, there was an opportunity to provide input or feedback via an online survey. For more information on the stakeholders participating in the consultation process, see Appendix B.
The consultation processes engaged stakeholders to:
- consider what has changed in the context of Aboriginal and Torres Strait Islander health and
- medical research and health outcomes since the release of Road Map 1
- think critically about the strengths and achievements of Road Maps 1 and 2, as well as the opportunities for improvement
- test and refine the objective for Road Map 3
- discuss ideas for research priority areas for Road Map 3
- generate insights on how NHMRC can continue to engage with Aboriginal and Torres Strait Islander communities and health and medical researchers and strengthen the Aboriginal and Torres Strait Islander health research sector.
Figure 2 below presents the key themes that emerged from the workshop consultations.2 A more detailed description on each of these themes follows.
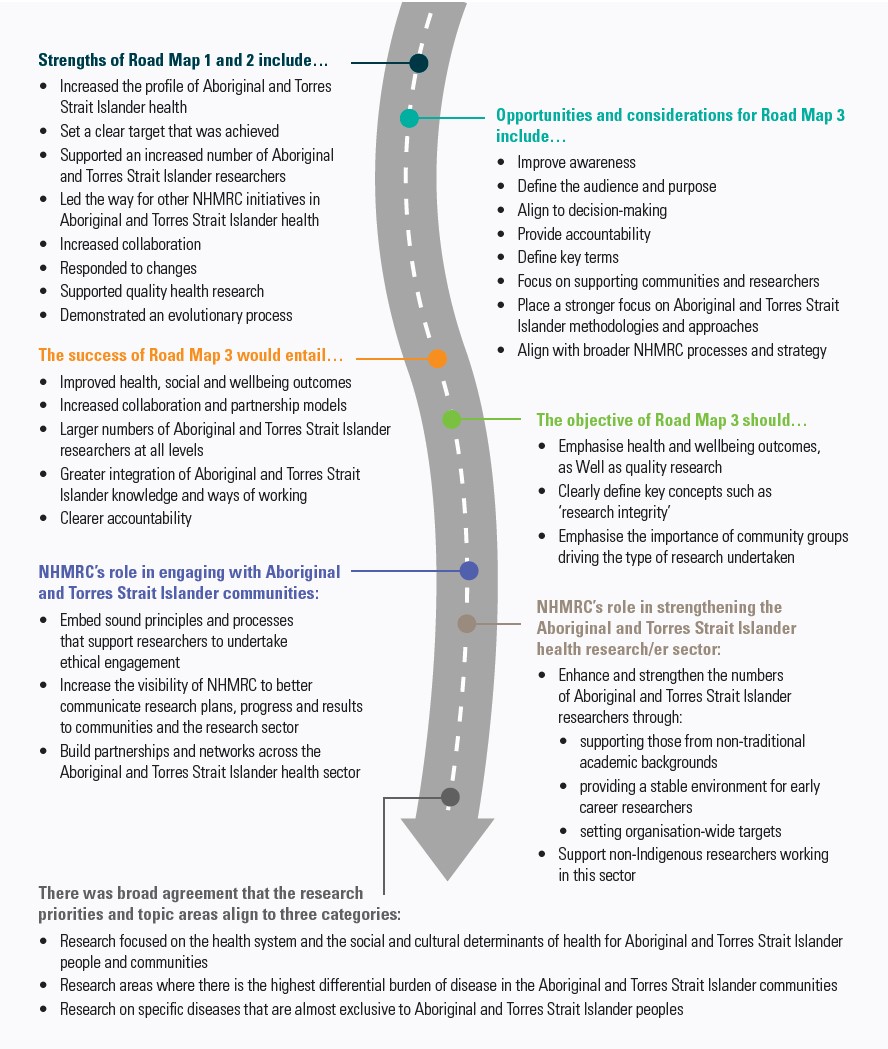
- Image description - Figure 2
Strengths of Road Map 1 and 2 include…
- Increased the profile of Aboriginal and Torres Strait Islander health
- Set a clear target that was achieved
- Supported an increased number of Aboriginal and Torres Strait Islander researchers
- Led the way for other NHMRC initiatives in Aboriginal and Torres Strait Islander health
- Increased collaboration
- Responded to changes
- Supported quality health research
- Demonstrated an evolutionary process
Opportunities and considerations for Road Map 3 include…
- Improve awareness
- Define the audience and purpose
- Align to decision-making
- Provide accountability
- Define key terms
- Focus on supporting communities and researchers
- Place a stronger focus on Aboriginal and Torres Strait Islander methodologies and approaches
- Align with broader NHMRC processes and strategy
The success of Road Map 3 would entail…
- Improved health, social and wellbeing outcomes
- Increased collaboration and partnership models
- Larger numbers of Aboriginal and Torres Strait Islander researchers at all levels
- Greater integration of Aboriginal and Torres Strait Islander knowledge and ways of working
- Clearer accountability
The objective of Road Map 3 should…
- Emphasise health and wellbeing outcomes, as Well as quality research
- Clearly define key concepts such as ‘research integrity’
- Emphasise the importance of community groups driving the type of research undertaken
NHMRC’s role in engaging with Aboriginal and Torres Strait Islander communities:
- Embed sound principles and processes that support researchers to undertake ethical engagement
- Increase the visibility of NHMRC to better communicate research plans, progress and results to communities and the research sector
- Build partnerships and networks across the Aboriginal and Torres Strait Islander health sector
NHMRC’s role in strengthening the Aboriginal and Torres Strait Islander health research/er sector:
- Enhance and strengthen the numbers of Aboriginal and Torres Strait Islander researchers through:
- supporting those from non-traditional academic backgrounds
- providing a stable environment for early career researchers
- setting organisation-wide targets
- Support non-Indigenous researchers working in this sector
There was broad agreement that the research priorities and topic areas align to three categories:
- Research focused on the health system and the social and cultural determinants of health for Aboriginal and Torres Strait Islander people and communities
- Research areas where there is the highest differential burden of disease in the Aboriginal and Torres Strait Islander communities
- Research on specific diseases that are almost exclusive to Aboriginal and Torres Strait Islander peoples
Key themes from the Road Map 3 national consultation
Throughout the course of the seven workshops and online consultation, participants were asked to share their perspectives on the following questions:
- What were the strengths of Road Maps 1 and 2 and what were the areas for improvement?
- What would success look like for Road Map 3?
- What should be the objective of Road Map 3?
- What is the role of NHMRC in engaging with Aboriginal and Torres Strait Islander communities?
- What is the role of NHMRC in strengthening the Aboriginal and Torres Strait Islander health research/er sector?
- What should be the research priorities or focus areas of Road Map 3?
Interviews with representatives from Aboriginal and Torres Strait Islander health research and peak bodies covered a similar range of topics. Their views relating to the key themes are incorporated.
This section summarises the key themes that emerged from the discussion around each of these questions. Feedback or discussion on areas outside of this scope was documented separately.
1 What were the strengths and areas for improvement in Road Maps 1 and 2?
During the workshops participants considered the changes in Aboriginal and Torres Strait Islander health in recent years and provided feedback on Road Maps 1 and 2. Participants reported on the strengths of the previous Road Maps, as well as what could be improved for Road Map 3. There were many common insights and themes across the seven workshops.

- Image description - Figure 3
Strength of Roads Map 1 and 2:
- Increased the profile of Aboriginal and Torres Strait Islander health
- Set a clear target that was achieved
- Supported an increased number of Aboriginal and Torres Strait Islander researchers
- Led the way for other NHMRC initiatives in Aboriginal and Torres Strait Islander health
- Increased collaboration in the sector
- Responded to changes in research priorities
- Embodied principles that supported quality Aboriginal and Torres Strait Islander health research
- Demonstrated an evolutionary process
Opportunities and considerations for Road Map 3:
- Define the purpose and audience
- Improve the awareness of Road Map 3 outside the Aboriginal and Torres Strait Islander health sector
- Align Road Map 3 to NHMRC decision making
- Provide accountability for funding decisions and communicate impact where possible
- Define what is included in ‘Aboriginal and Torres Strait Islander health research’
- Focus on supporting communities
- Place a stronger focus on Aboriginal and Torres Strait Islander methodologies and approaches, including in evaluation and research translation
- Align with broader NHMRC processes and strategy
Eight key strengths of Road Maps 1 and 2 were identified through the consultation process
Consultation participants identified a number of key strengths of Road Maps 1 and 2. Feedback was collated and synthesised into eight key strengths:
- Increased the profile of Aboriginal and Torres Strait Islander health – across the workshops stakeholders commended the Road Maps for increasing the profile of Aboriginal and Torres Strait Islander health research. The Road Maps also supported placing Aboriginal and Torres Strait Islander health on the national agenda through a clear commitment by a Commonwealth agency. This demonstrated leadership in the area by NHMRC.
- Set a clear target that was achieved – stakeholders supported the clear target for funds allocation, with the target of 5% of research funding directed towards Aboriginal and Torres Strait Islander heath projects.3 In addition, achievement of this target in recent years (including the achievement of 6.3% in 2015-2016) was also seen as a significant strength of the Road Maps.
- Supported an increased number of Aboriginal and Torres Strait Islander researchers – stakeholders commented that the Road Maps supported an increase in the number of Aboriginal and Torres Strait Islander health researchers by promoting Aboriginal and Torres Strait Islander health as a discipline.
- Led the way for other NHMRC initiatives in Aboriginal and Torres Strait Islander health – this includes Targeted Calls for Research (TCR) and priority driven research on Aboriginal and Torres Strait Islander health outcomes, which occurred separate to Road Maps 1 and 2.
- Increased collaboration in the sector – participants reported that Road Maps supported and enabled improved engagement with peak bodies and raised the consciousness and importance of collaboration with government on Aboriginal and Torres Strait Islander health research.
- Responded to changes in research priorities – Road Maps 1 and 2 supported a shift in the types of health research that were funded with a shift from biomedical focused research to a broader research focus, including public health and preventative health. At a high level, it also ensured that funding was more closely aligned with priorities.
- Embodied principles that supported quality Aboriginal and Torres Strait Islander health research – stakeholders offered positive feedback that the underlying principles of Road Maps 1 and 2 provided a clear articulation of a holistic view of health, promoted appropriate research practice, and supported active participation of Aboriginal and Torres Strait Islander communities and researchers.
- Demonstrated an evolutionary process – participants noted that the Road Map process had a sustained focus with multiple touch points over the past 10 years. This contrasted positively with other strategic programs. Participants complimented NHMRC on the clear evolution from Road
- Map 1 to Road Map 2, and the current evolution to Road Map 3.
Participants identified opportunities for improvement that can guide development of Road Map 3
Participants were asked to provide feedback on the opportunities to improve the previous Road Map documents. This provides valuable input for the development of Road Map 3. The identified opportunities include:
- Improve the awareness of Road Map 3 outside the Aboriginal and Torres Strait Islander health sector – despite the fact that there was increased awareness within the Aboriginal and Torres Strait Islander research community, participants felt that awareness, value and familiarity of
- the Road Maps could be enhanced.
- Define the audience and purpose of Road Map 3 – some stakeholders commented that the purpose and audiences of Road Maps 1 and 2 were a little unclear. Road Map 3 should clearly communicate the purpose of the document and who is the intended audience.
- Align Road Map 3 to NHMRC decision-making – alignment of the Road Maps to internal NHMRC decision-making could be improved. For example, it was not apparent in funding investment decisions whether the funding provided aligned to research priorities outlined in the
- previous Road Map documents. Road Map 3 should clearly align to decision-making processes within the organisation.
- Provide accountability for funding decisions and communicate impact where possible – participants reflected on the limited information available to understand what Aboriginal and Torres Strait Islander health projects and priority areas are funded by NHMRC. They suggested that where possible, Road Map 3 should support greater communication processes around the level of investments for projects/priority areas and the impact of investments on communities and health outcomes.
- Define what is included in 'Aboriginal and Torres Strait Islander health research' – not all participants were clear on what was included in NHMRC definition of 'Aboriginal and Torres Strait Islander health research'. They asked if it reflected the focus of the research, the background of the researchers, or both. Others commented that it was unclear what was included in the 5% investment target set by NHMRC. Road Map 3 should clearly outline what represents Aboriginal and Torres Strait Islander health research and set distinct targets for the number of Aboriginal and Torres Strait Islander researchers and Aboriginal and Torres Strait Islander-focused research projects.
- Focus on supporting communities and researchers – Road Maps 1 and 2 targets have a strong focus on Aboriginal and Torres Strait Islander research through the 5% target, but have less of a clear focus on capacity and supporting Aboriginal and Torres Strait Islander researchers. There is an opportunity for Road Map 3 to place a greater emphasis on supporting Aboriginal and Torres Strait Islander researchers and establishing key targets to support this.
- Place a stronger focus on Aboriginal and Torres Strait Islander methodologies and approaches, including in evaluation and research translation – feedback was provided that there was not a strong focus on evaluation, research translation or Indigenous approaches within the previous Road Map documents. Stakeholders commented that there was an opportunity for a greater emphasis on these and their benefits in Road Map 3.
- Align with broader NHMRC processes and strategy – participants suggested that alignment with key NHMRC processes would strengthen the impact of Road Map 3.
2 What would success look like for Road Map 3?
At the beginning of the workshops, stakeholders reflected on the question, ‘What would success look like for Road Map 3?’ Their answers considered both the process by which Road Map 3 should be developed and implemented, as well as the outcomes they hoped to see if Road Map 3 was successful. Across all workshop locations and individual conversations, the statements on success generally centered around five main areas. A brief description is provided in Figure 4. Workshop participants continually raised these areas during the workshop as pivotal parts of Road Map 3.
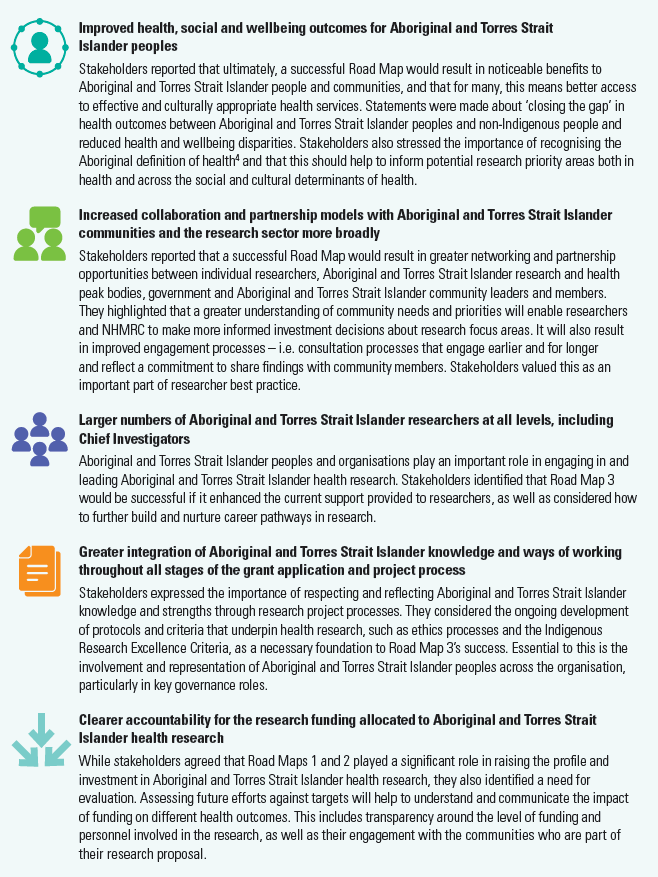
- Image description - Figure 4
Improved health, social and wellbeing outcomes for Aboriginal and Torres Strait Islander peoples
Stakeholders reported that ultimately, a successful Road Map would result in noticeable benefits to Aboriginal and Torres Strait Islander people and communities, and that for many, this means better access to effective and culturally appropriate health services. Statements were made about ‘closing the gap’ in health outcomes between Aboriginal and Torres Strait Islander peoples and non-Indigenous people and reduced health and wellbeing disparities. Stakeholders also stressed the importance of recognising the Aboriginal definition of health4 and that this should help to inform potential research priority areas both in health and across the social and cultural determinants of health.
Increased collaboration and partnership models with Aboriginal and Torres Strait Islander communities and the research sector more broadly
Stakeholders reported that a successful Road Map would result in greater networking and partnership opportunities between individual researchers, Aboriginal and Torres Strait Islander research and health peak bodies, government and Aboriginal and Torres Strait Islander community leaders and members. They highlighted that a greater understanding of community needs and priorities will enable researchers and NHMRC to make more informed investment decisions about research focus areas. It will also result in improved engagement processes – i.e. consultation processes that engage earlier and for longer and reflect a commitment to share findings with community members. Stakeholders valued this as an important part of researcher best practice.
Larger numbers of Aboriginal and Torres Strait Islander researchers at all levels, including Chief Investigators
Aboriginal and Torres Strait Islander peoples and organisations play an important role in engaging in and leading Aboriginal and Torres Strait Islander health research. Stakeholders identified that Road Map 3 would be successful if it enhanced the current support provided to researchers, as well as considered how to further build and nurture career pathways in research.
Greater integration of Aboriginal and Torres Strait Islander knowledge and ways of working throughout all stages of the grant application and project process
Stakeholders expressed the importance of respecting and reflecting Aboriginal and Torres Strait Islander knowledge and strengths through research project processes. They considered the ongoing development of protocols and criteria that underpin health research, such as ethics processes and the Indigenous Research Excellence Criteria, as a necessary foundation to Road Map 3’s success. Essential to this is the involvement and representation of Aboriginal and Torres Strait Islander peoples across the organisation, particularly in key governance roles.
Clearer accountability for the research funding allocated to Aboriginal and Torres Strait Islander health research
While stakeholders agreed that Road Maps 1 and 2 played a significant role in raising the profile and investment in Aboriginal and Torres Strait Islander health research, they also identified a need for evaluation. Assessing future efforts against targets will help to understand and communicate the impact of funding on different health outcomes. This includes transparency around the level of funding and personnel involved in the research, as well as their engagement with the communities who are part of their research proposal.
3 What should be the objective of Road Map 3?
Consultation participants provided feedback on the following draft objective for Road Map 3: To support NHMRC to improve Aboriginal and Torres Strait Islander health and wellbeing outcomes by ensuring research integrity and outlining research priorities that reflect community preferences and the national health context.
Overall feedback indicated that this objective is heading in the right direction due to its emphasis on improving health and wellbeing outcomes, as well as quality research. Participants recommended considering the following changes:
- Review the expression, 'outlining research priorities that reflect community preferences', so that there is a greater emphasis on community groups defining and driving the type of research undertaken.
- Consider changing 'national health context' to 'national priorities'. For greater simplicity, one stakeholder proposed 'community and national priorities' instead of 'priorities that reflect community preferences and the national health context'.
- Define 'research integrity' so that it is clear that it reflects quality research, ethically-sound research and research that results in benefits for Aboriginal and Torres Strait Islander peoples.
- Take into account the option of emphasising improved health outcomes in the context of social and cultural determinants of health.
- Consider including some text around investment in Aboriginal and Torres Strait Islander researchers.
Participants in one of the workshops expressed a clear preference against using the concept of 'closing the gap' as had been used in Road Map 2. It was not felt that this was the correct terminology and language for Road Map 3 as it reflected a deficit approach.
One stakeholder group proposed the following objective as an alternative: To support high quality research that produces strong evidence that will contribute to improving Aboriginal and Torres Strait Islander health and wellbeing outcomes.
The final objective for Road Map 3 will reflect the objectives tested throughout the workshop and the feedback noted above, as well as feedback provided during public consultation.
4 What is the role of NHMRC in engaging with Aboriginal and Torres Strait Islander communities?
All stakeholders agreed that ethical and appropriate engagement with communities is essential to identifying health research topics that reflect community needs and priorities. This type of engagement also supports the successful delivery of projects that result in benefits and health improvements for Aboriginal and Torres Strait Islander people and communities.
Workshop participants identified NHMRC's role in engaging with Aboriginal and Torres Strait Islander communities as threefold:
- Embed sound principles and processes that support researchers to undertake ethical engagement
- Increase the visibility of NHMRC to better communicate research plans, progress and results to communities and the research sector
- Build partnerships and networks across the Aboriginal and Torres Strait Islander health sector. Each of these is explored in more detail below.
Embed sound principles and processes that support researchers to undertake ethical engagement
NHMRC is strongly committed to engaging with Aboriginal and Torres Strait Islander communities. This is reflected in the establishment of the PCIC and the development of a range of protocols and guiding documents that shape the process for research grant applications and project development, such as the Values and Ethics Guidelines, Keeping Research on Track, and the Indigenous Research Excellence Criteria. It is also supported by the principles that have underpinned both Road Maps 1 and 2, which include ethical practices and community involvement as a priority in the development, conduct and communication of research.
Throughout the workshops, participants reported that NHMRC could better support researchers to undertake ethical engagement and research by more clearly aligning key NHMRC documents and protocols (Values and Ethics Guidelines, Keeping Research on Track, the Indigenous Research Excellence Criteria) to Road Map 3 and integrating them more strongly into NHMRC's grant and assessment procedures. Stakeholders suggested that increasing the Aboriginal and Torres Strait Islander representation on all NHMRC Human Research Ethics Committees could also play an important role in supporting ethical engagement and research.

Stakeholders emphasised the importance of the Indigenous Research Excellence Criteria to the grant application and assessment process. The criteria are:
- Community engagement – demonstrating how potential outcomes are a priority for Aboriginal and Torres Strait Islander communities
- Benefit – through addressing an important health issue for Aboriginal and Torres Strait Islander peoples
- Sustainability and transferability – showing how the project has the potential to lead to achievable and effective contributions to health gains beyond the life of the project
- Building capability – showing how Aboriginal and Torres Strait Islander people, communities and researchers will develop relevant capabilities through partnership and participation.
However, stakeholders also called for greater clarity around how they are defined and applied by review committees throughout the grant application process. In particular, they highlighted the importance of defining 'Research Excellence' and the four criteria from an Aboriginal and Torres Strait Islander perspective. Stakeholders also felt that the definition of whether a project qualifies as Aboriginal and Torres Strait Islander health research is currently too ambiguous and could be tighter with stronger and more ambitious targets.5 Stakeholders at a number of the workshops suggested that NHMRC could consider adopting the principles that the Lowitja Institute identifies as underpinning their approach to research:
- Beneficence – to act for the benefit of Aboriginal and Torres Strait Islander peoples in the conduct of our research
- Leadership by Aboriginal and Torres Strait Islander peoples
- Engagement of research end users (Aboriginal and Torres Strait Islander organisations and communities, policymakers, other potential research users)
- Development of the Aboriginal and Torres Strait Islander research workforce
- Measurement of impact in improving Aboriginal and Torres Strait Islander peoples’ health.6
Stakeholders also identified that NHMRC could better advocate and hold researchers to account by ensuring that they regularly communicate with the communities they are working with throughout all stages of the project lifecycle. In particular, many stakeholders noted that researchers do not sufficiently engage with Aboriginal and Torres Strait Islander communities at the end of a research project to report on the project's outcomes and the impact of the community involved. This is an important step as the purpose of the research should be to bring a positive outcome for the community (e.g. improve health outcomes or access to health services). Another role that NHMRC could play in engaging with communities is providing clearer guidance for communities about the research process, including what they can expect from researchers. For example, NHMRC could include the option of co-ownership of intellectual property between researchers and Aboriginal and Torres Strait Islander communities in guidelines as one mechanism to support positive community engagement.
Stakeholders also raised concerns regarding the processes for NHMRC's Targeted Calls for Research (TCRs). They proposed a review of the current timeframe and investment provided to TCR grants so that researchers have a more appropriate lead time to engage with communities. The current six-week timeframe was not deemed sufficient for meaningful engagement. NHMRC acknowledged this issue and noted they had extended the timeframes for a recent TCR in response.
Lastly, stakeholders perceive ongoing relationships with local communities as incredibly important, but stated that they do not currently have the financial or other supports to invest time in these relationships. Without sustainable relationship development, instances of 'fly-in fly-out' researchers, who have not established trust with communities, are likely to continue.
Increase the visibility of NHMRC to better communicate research plans, progress and results to communities and the research sector
Throughout the consultations, stakeholders called for clearer and more regular reporting around research priorities, funding allocations and progress towards targets. NHMRC is a national body with a wide network including government, health professionals, researchers, higher education bodies and universities, research organisations, and Aboriginal Community Controlled Health Organisations.
Stakeholders identified multiple opportunities for NHMRC to proactively communicate its role, activities and achievements in the context of Aboriginal and Torres Strait Islander health research to these stakeholders.
Consultation participants recognised that promoting NHMRC’s achievements and vision would help to generate further engagement across key stakeholder groups, identify potential new partnerships, bring about a greater level of transparency across the organisation and sector, and build the awareness, value and reputation of Road Map 3.
Some of the opportunities identified included:
- increasing NHMRC's presence on social media, building on NHMRC accounts on Facebook, Twitter and LinkedIn
- a Road Map 'dashboard' on NHMRC website
- regular updates on progress towards Road Map 3 targets in other mediums such as newsletters, emails, blogs and online videos.
Build partnerships and networks across the Aboriginal and Torres Strait Islander health sector
Stakeholders expressed the importance of NHMRC consulting widely, and also deeply, but acknowledged that this is challenging for NHMRC to do alone. They recommended that NHMRC focus on continuing to build partnerships with key stakeholder groups including health peak bodies, educational institutions, health practitioners, government departments and policy agencies at national, state and local levels.
Through this process, NHMRC will have a greater understanding of community priorities as well as the opportunities for project collaboration and activities related to sector-wide capacity building. It will also enable NHMRC to align its work in Aboriginal and Torres Strait Islander health with other strategies and initiatives.
5 What is the role of NHMRC in strengthening the Aboriginal and Torres Strait Islander health research/er sector?
Throughout the consultation process, participants were clear that as the national body for health and medical research, NHMRC plays an important role in facilitating the strengthening of researchers and driving high quality research in Aboriginal and Torres Strait Islander health. The following sub‑sections provide detail on the types of initiatives raised by stakeholders to enhance and strengthen the numbers of Aboriginal and Torres Strait Islander researchers, and to enhance the cultural capability of non- Indigenous researchers working in the sector.
Initiatives proposed to enhance and strengthen the numbers of Aboriginal and Torres Strait Islander researchers
Participants expressed a clear desire for NHMRC to have a stronger focus on supporting and developing Aboriginal and Torres Strait Islander researchers. A past initiative to support Aboriginal and Torres Strait Islander researchers was the Building Indigenous Researcher Capacity grants. NHMRC's Rising Star Award, which is awarded to the highest ranked application by an Aboriginal and Torres Strait Islander researcher in the Early Career Fellowship scheme, is also a current initiative that is well received.
Stakeholders commended these initiatives but felt there was further opportunity to support Aboriginal and Torres Strait Islander researchers. In particular, participants outlined that support was required to promote and support doctoral students transitioning into post-doctoral research positions.
Some workshops more fully explored the theme of building Aboriginal and Torres Strait Islander researchers, discussing the ways in which a more level playing field could be achieved.
Many stakeholders considered that NHMRC could play a valuable role in supporting early career researchers through communicating the different career options available for Aboriginal and Torres Strait Islander researchers. Feedback related to three areas:
- supporting researchers from non-traditional academic backgrounds
- providing a stable environment for early career researchers
- setting organisation-wide targets to build the cohort of Aboriginal and Torres Strait Islander researchers.
Supporting researchers from non-traditional academic backgrounds: Participants were clear that NHMRC should proactively recognise and support researchers who come from non-traditional academic pathways into health research positions. In the Aboriginal and Torres Strait Islander health research sector a significant number of Aboriginal and Torres Strait Islander researchers come from a practitioner background, such as nurses or Aboriginal health workers, as opposed to an academic pathway (from undergraduate to doctorate and through a post-doctoral research position).
Participants highlighted some of the challenges that researchers from non-traditional academic pathways can face. For example, demonstrating track record is difficult with limited research experience/ outputs. Participants stated that NHMRC could place greater emphasis on the practical experience of researchers from these backgrounds. This may include a grants funding criterion such as ‘demonstrated community engagement’ or access to fellowships for researchers from non‑traditional academic backgrounds. Participants also noted that NHMRC could play a role in supporting individuals who balance research with other roles, such as health practitioners.
Providing a stable environment for early career researchers: Many stakeholders suggested that NHMRC could work in partnerships with universities to provide a more stable and supportive environment for researchers. This could include funding cohorts of Aboriginal and Torres Strait Islander doctoral and post-doctoral researchers at universities with mentoring support to ensure appropriate networks and structures are in place for early career researchers.
Setting organisation-wide targets to build the cohort of Aboriginal and Torres Strait Islander researchers: A large number of stakeholders reported on the importance of continuing to set targets for the number of Aboriginal and Torres Strait Islander researchers who receive NHMRC grants. It was recommended that these targets align with NHMRC’s new grant program. The new grant program will be comprised of fours streams—Investigator grants, Synergy grants, Ideas grants, and Strategic and Leveraging grants. (Further information about the new grant program is here).
Across all the consultation workshops and interviews, stakeholders raised the importance of accountability to targets and further stated that NHMRC should communicate progress towards targets and outcomes on a regular basis (e.g. every three years). This will help ensure that NHMRC has a strong understanding about what initiatives are (or are not) working to increase and support the number of Aboriginal and Torres Strait Islander researchers.
Support for non-Indigenous researchers working in this sector
Stakeholders highlighted that NHMRC could also play a role in supporting non-Indigenous researchers who are working with Aboriginal or Torres Strait Islander communities and working on Aboriginal and Torres Strait Islander health projects. Some participants felt that NHMRC could encourage non-Indigenous researchers to collaborate more strongly and meaningfully with Indigenous researchers. Non-Indigenous researchers could engage Indigenous researchers as collaborators rather than junior research assistants. Participants were supportive of NHMRC’s current efforts, such as the provision of guidelines for working with Aboriginal and Torres Strait Islander communities, as well as sharing best practice and communicating principles. However feedback indicated that more could be done to promote strong cultural competence and safety.
Some ideas raised by participants included establishing more formalised expectations for engaging meaningfully with Aboriginal and Torres Strait Islander communities and supporting ‘community advisors’ to train researchers on Indigenous approaches to research. They considered it would be critical to have Aboriginal and Torres Strait Islander input on such guidelines, and include best practice examples or case studies.
6 What should be the research priorities or focus areas of Road Map 3?
Building on the initial consultations undertaken as part of the development of Road Map 3, a framework was proposed in the workshops to structure potential research priorities. This is depicted below in Figure 6.
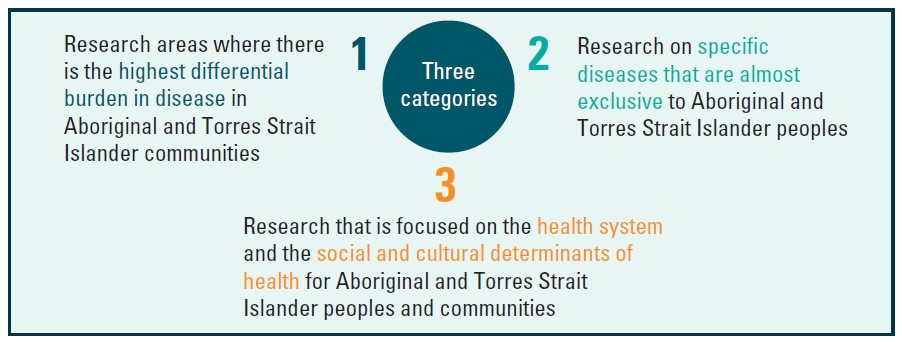
- Image description - Figure 6
Three categories:
- Research areas where there is the highest differential burden in disease in Aboriginal and Torres Strait Islander communities
- Research on specific diseases that are almost exclusive to Aboriginal and Torres Strait Islander peoples
- Research that is focused on the health system and the social and cultural determinants of health for Aboriginal and Torres Strait Islander peoples in communities.
At each of the workshops, stakeholders were asked to provide their insights on the research priorities for Road Map 3. A voting exercise grouped the research areas and showed participants which topics were considered most important for Road Map 3.
After testing the framework with stakeholders, there was broad agreement that the research priorities and topic areas aligned to the three categories in the framework, with some small modifications.
The three categories are discussed below, with information provided on the specific research topics that were identified under each.
1 Research areas where there is the highest differential burden of disease in the Aboriginal and Torres Strait Islander communities
Participants identified several research priorities focused on areas of the greatest differential burden of disease between Aboriginal and Torres Strait Islander peoples and other Australians. Research projects in this area should be predominately focused on Aboriginal and Torres Strait Islander communities.
There was also support for research projects that were focused on applied research and translation in Aboriginal and Torres Strait Islander communities or for Aboriginal and Torres Strait Islander populations.
Key themes from the discussions included:
- Mental health and social and emotional wellbeing (SEWB) – there was a strong focus on mental health and SEWB. In particular, there was an emphasis on research related to suicide prevention, particularly for young people. Other research topics such as substance abuse, addiction, bullying and self-harm were also identified as important.
- Chronic physical health conditions – participants indicated several chronic health conditions such as various forms of cancer, diabetes, kidney health, respiratory disease and cardiovascular disease. Research in all of these areas was seen as a high priority.
- Tuberculosis prevention – raised by participants from the Thursday Island workshop, with a particular emphasis on cross-border prevention.
- Vector borne diseases strategy – raised by participants from the Thursday Island workshop, including management of diseases such as malaria, Ross River Fever and other infectious diseases transmitted to humans.
Other conditions raised during broader consultations included palliative care, sexually transmitted infections and health of people with a disability.
Participants in one of the workshop locations proposed adjusting the theme to focus on research areas where there is the highest “differential quality of life” as opposed to the “differential burden of disease”. This would place a greater emphasis on early childhood and healthy ageing, where there can be a differential quality of life for Aboriginal and Torres Strait Islander peoples without a burden of disease necessarily existing.
2 Research on specific diseases that are almost exclusive to Aboriginal and Torres Strait Islander peoples. Throughout the consultation process, stakeholders also identified research on specific diseases that are almost exclusive to Aboriginal and Torres Strait Islander peoples and communities.
These included:
- Acute Renal Failure
- Rheumatic Heart Disease
- Eye and ear health
- Vector borne infectious diseases, particularly in the Torres Strait.
Feedback related to this category was more limited than the other two. However, participants did reflect that specific diseases almost exclusive to Aboriginal and Torres Strait Islander peoples represented an important focus. They considered it important to direct research funds to these conditions.
3 Research focused on the health system and the social and cultural determinants of health for Aboriginal and Torres Strait Islander peoples and communities
Out of the three research categories, support from participants was strongest for research priorities that align with the health system and social and cultural determinants of health. There was strong support for research that focused on understanding the effectiveness of the health system for
Aboriginal and Torres Strait Islander peoples. There was also a strong preventative focus, with public health research emphasised across the workshop sessions. Participants suggested that within this category there should also be a focus on applied research such as intervention studies and risk studies in Aboriginal and Torres Strait Islander communities.
Key themes from the discussions included:
- Health across the lifecycle – there was strong support for health research that focused across the human lifecycle, with a particular focus on childhood, adolescence, and healthy ageing. In addition, there was also an emphasis on intergenerational health, including early childhood health and development, and maternal health.
- Public health and preventative disease – preventing disease through awareness, early intervention and public health campaigns was identified as a key priority. Stakeholders highlighted an interest in research focused on assessing health promotion activities and interventions in Aboriginal and Torres Strait Islander communities or targeted to Aboriginal and Torres Strait Islander communities.
- Social determinants of health – there was strong and consistent support for research focused on the wide range of social determinants of health that influence differences in health status for Aboriginal and Torres Strait Islander peoples and communities. Specific examples included housing, and domestic and family violence. Health determinants and outcomes for people who are incarcerated were also identified as a research priority.
- Culture and Aboriginal and Torres Strait Islander health – the centrality of culture to Aboriginal and Torres Strait Islander health was identified as critically important. Research that utilises a strengths based approach and identifies the value of Aboriginal and Torres Strait Islander culture on health outcomes was supported. Resilience represents one component of this.
- The health system – there was a strong focus on assessing Aboriginal and Torres Strait Islander people’s interaction and experience accessing the mainstream health system. In addition, understanding the effectiveness of community controlled and other models of care through research was seen as a priority. Integration of data sources and improving data linkages was also identified as a research priority related to the functioning of the health system.
- Cultural competence, cultural safety and racism – There was a clear focus on cultural competence, safety and racism within the mainstream health system in many of the workshop locations. There was a particular focus on systemic and institutionalised racism and the lack of cultural responsiveness of health professionals, and the subsequent impact this has on health outcomes. It should be noted that this was not identified as a key research priority in the Thursday Island workshop.
Some of the research priorities identified did not strongly align with the categories in the proposed framework
Personalised health care and genomics were two areas raised by participants in one of the workshops that do not clearly align with the proposed framework. These participants recognised and communicated that advances in personal health care and advances in fields related to genomics will be increasingly critical to the improvement of health outcomes for Aboriginal and Torres Strait Islander peoples and communities.
Some participants also suggested that research priorities could be geographically focused. For example, some stakeholders outlined that geographic areas such as the Torres Strait and Tasmania require a distinct focus and therefore the priorities for those areas should be considered separately.
During the workshops NHMRC acknowledged the cultural and health priority differences between all regions and emphasised that Road Map 3 will reflect on the differences that exist between different Aboriginal and Torres Strait Islander communities, while still clearly communicating common issues and opportunities that exist across them.
Targeted Calls for Research may supplement the priorities outlined in Road Map 3
It is intended that Road Map 3 will be a living document that will respond to, and be continually informed by, community input. Stakeholders strongly supported TCRs due to their role in driving research in new areas that are identified as vitally important. This approach provides one mechanism NHMRC can use to address emerging research issues in Aboriginal and Torres Strait Islander health that have not previously been identified.
Furthermore NHMRC may wish to use TCRs to provide a mechanism for prioritising research areas that have not received significant levels of funding to date through the broader grants program. Monitoring the funding allocated to each of the three research categories outlined in Figure 6 will be important to assess, which areas have been covered in each funding round, and where a TCR might be valuable.
Footnotes
1 Appendix A provides background information on the role of NHMRC and the PCIC.
2 The workshop consultations built on the themes identified in the initial interview consultations.
3 NHMRC has a commitment to spend at least 5% of funding under the Medical Research Endowment Account on Aboriginal and Torres Strait Islander health each year; NHMRC 2017, accessed online, available at: Aboriginal and Torres Strait Islander health.
4 The Aboriginal definition of health includes the social, emotional and cultural wellbeing of the whole Community in which each individual is able to achieve their full potential as a human being thereby bringing about the total wellbeing of their Community. National Aboriginal Health Strategy, 1989.
5 To qualify as Aboriginal and/or Torres Strait Islander health research, NHMRC Funding Rules state that “at least 20% of the research effort and/or capacity building must relate to Aboriginal and/or Torres Strait Islander health.”
6 Lowitja Institute (2017), Annual Report 2016, accessed online, available at: http://www.lowitja.org.au/sites/default/files/docs/Lowitja-Inst-AR2016.pdf
Appendix A: The role of NHMRC and PCIC
The role of NHMRC
NHMRC has been the Australian government body for supporting health and medical research since 1937. The principal functions of the organisation are to foster improved health and medical knowledge through:
- funding research and translating research findings into evidence-based clinical practice
- administering legislation governing research
- issuing guidelines and advice for ethics in health
- promoting public health.
On behalf of the Australian Government, NHMRC is the leading national investor in health and medical research, advancing health and medical knowledge to improve the health of all Australians.
The organisation develops evidence-based health advice for the Australian community, health professionals and governments, and provides advice on ethical practice in health care and the conduct of health and medical research.
The role of the PCIC
The PCIC provides advice to NHMRC Council and CEO on issues relating to Aboriginal and Torres Strait Islander health research according to its Terms of Reference, including the implementation of Road Map 2 and the development and implementation of Road Map 3.
The committee is comprised of Aboriginal and Torres Strait Islander representatives currently on NHMRC Council and Principal Committees, and early career researchers. Membership includes:
- Prof Sandra Eades (Chairperson and NHMRC Council Member)
- A/Prof Daniel McAullay (Research Committee & Australian Health Ethics Committee)
- Prof Yvonne Cadet-James (Health Translation Advisory Committee)
- A/Prof Kelvin Kong (Health Innovation Advisory Committee)
- Dr Yvette Roe, Early Career Researcher
- Dr Simon Graham, Early Career Researcher
- Mr Ali Drummond, Early Career Researcher
Appendix B: Workshop locations, participants and approach
The consultation process for Road Map 3 began in March 2017 and involved interviews with representatives from nine leading Aboriginal and Torres Strait Islander health and research peak bodies followed by workshops across Australia. More details on interviewees and workshop participants is included below.
Interviewees included:
- Ian Anderson, Department of Prime Minister and Cabinet
- Adrian Carsons and Carmel Nelson, Institute for Urban Indigenous Health
- Margaret Cashman, Aboriginal Health and Medical Research Council of NSW
- Kathleen Clapham, National Indigenous Research and Knowledges Network
- Craig Dukes, Australian Indigenous Doctors’ Association
- Mick Gooda, Royal Commission into the Child Protection and Youth Detention Systems of the Northern Territory
- Romlie Mokak, The Lowitja Institute Australia’s National Institute for Aboriginal and Torres Strait Islander Health Research
- Craig Ritchie, Australian Institute of Aboriginal and Torres Strait Islander Studies Pat Turner, National Aboriginal Community Controlled Health Organisation
NHMRC and PCIC, in partnership with Nous, facilitated the seven workshops across Australia. Workshop locations were:
- Adelaide (19 May)
- Darwin (30 May)
- Sydney (9 June)
- Perth (15 June)
- Brisbane (16 June)
- Melbourne (23 June)
- Thursday Island (17 July)
Locations were selected based on areas that are close to a range of research centres and other key stakeholders as well as geographic diversity. Locations for previous Road Map workshops also informed the choice of locations.
For those who were unable to attend the workshops, an online survey was provided to collect feedback on the questions that were asked during the workshops.
Participants across the workshops included:
- Aboriginal and Torres Strait Islander professional health bodies
- Aboriginal and Torres Strait Islander health sector experts and practitioners
- Health practitioners
- Relevant academic and research institutions
- Relevant government agencies
- Community members/health consumers
- NHMRC staff and PCIC representatives All workshops were facilitated by Nous
- A breakdown of participants at each workshop location is provided below.
A breakdown of participants at each workshop location is provided below.
| Name | Organisation |
|---|---|
| Gokhan Ayturk | Aboriginal Health Council of South Australia |
| Lisa Moutzouris | Australian Bureau of Statistics |
| Dennis McDermott | Flinders University |
| Alan Singh | NHMRC |
| Naomi Gowor | NHMRC |
| Sam Faulkner | NHMRC |
| Tony Kingdon | NHMRC |
| Michelle Kealy | Nunkuwarrin Yunti of South Australia Inc |
| Dan McAullay | PCIC, NHMRC |
| Yvette Roe | PCIC, NHMRC |
| Nicola Spurrier | South Australia Health |
| Paddy Phillips | South Australia Health |
| Andrea McKivett | South Australia Health and Medical Research Institute |
| David Banham | South Australia Health and Medical Research Institute |
| James Ward | South Australia Health and Medical Research Institute |
| Janet Kelly | South Australia Health and Medical Research Institute |
| Jessica Reid | South Australia Health and Medical Research Institute |
| Karen Glover | South Australia Health and Medical Research Institute |
| Karen Laverty | South Australia Health and Medical Research Institute |
| Kim Morey | South Australia Health and Medical Research Institute |
| Leda Sivak | South Australia Health and Medical Research Institute |
| Natalie Bauer | South Australia Health and Medical Research Institute |
| Odette Gibson | South Australia Health and Medical Research Institute |
| Steve Wesselingh | South Australia Health and Medical Research Institute |
| Wendy Keech | South Australia Health and Medical Research Institute |
| Dylan Coleman | University of Adelaide |
| Margaret Scrimgeour | University of Adelaide |
| Shane Hearn | University of Adelaide |
| Terry Dunbar | University of Adelaide |
| Angela Brown | University of South Australia |
| Natasha Howard | University of South Australia |
| Ian Olver | University of South Australia |
| Name | Organisation |
|---|---|
| Patricia Elarde | Diabetes Queensland |
| Alison Rice | Griffith University |
| Kyly Mills | Griffith University |
| Tina Skinner-Adams | Griffith University |
| Connie Archer | Indigenous Affairs Group, Department of the Prime Minister and Cabinet |
| Donisha Duff | Kidney Health Australia |
| Gail Garvey | Menzies School of Health Research |
| Lisa Whop | Menzies School of Health Research |
| Alan Singh | NHMRC |
| Sam Faulkner | NHMRC |
| Tony Kingdon | NHMRC |
| Ali Drummond | PCIC, NHMRC |
| Yvonne Cadet-James | PCIC, NHMRC |
| Alex Kathage | QLD Health |
| Kathy Brown | QLD Health |
| Sue Hooper | QLD Health |
| Ray Mahoney | QLD University of Technology |
| Vicki Slinko | Queensland Aboriginal and Islander Health Council |
| Name | Organisation |
|---|---|
| Karrina Demasi | Aboriginal Medical Services Alliance Northern Territory |
| John Guenther | Batchelor Institute |
| Peter Stephenson | Batchelor Institute |
| Tim Carey | Centre for Remote Health, Flinders University and Charles Darwin University |
| Sarah Ireland | Charles Darwin University |
| James Smith | Charles Darwin University |
| Kim Robertson | Charles Darwin University |
| Marilynne Kirshbaum | Charles Darwin University |
| Shane Motlop | Charles Darwin University |
| Joy McLoughlin | Danila Dilba Health Service |
| Rus Nasir | Department of Health |
| Tanja Hirvonen | Flinders University |
| Adam Thompson | Menzies School of Health Research |
| Alan Cass | Menzies School of Health Research |
| Chris Spargo | Menzies School of Health Research |
| Coralie Achterberg | Menzies School of Health Research |
| David Thomas | Menzies School of Health Research |
| Emily Bovill | Menzies School of Health Research |
| Karen Thomas | Menzies School of Health Research |
| Mark Mayo | Menzies School of Health Research |
| Matt Stevens | Menzies School of Health Research |
| Heather D’Antoine | Menzies School of Health Research |
| Alan Singh | NHMRC |
| Naomi Gowor | NHMRC |
| Sam Faulkner | NHMRC |
| Tony Kingdon | NHMRC |
| Sandra Eades | PCIC, NHMRC |
| Yvette Roe | PCIC, NHMRC |
| Yvonne Cadet-James | PCIC, NHMRC |
| Kalinda Griffiths | University of Sydney, Menzies and Charles Darwin University |
| Belinda Davis | University of Western Australia |
| Ruth Montgomery-Anderson | Visiting Scholar - Greenland |
| Name | Organisation |
|---|---|
| Fadwa Al-Yaman | Australian Institute of Health and Welfare |
| Jasmine Lyons | Centre for Health Equity, Melbourne School of Population and Global Health, University of Melbourne |
| Darren Clinch | Department of Health and Human Services |
| Shaun Lohear | Department of Health and Human Services |
| Romlie Mokak | Lowitja Institute |
| Bronte Spiteri | Lowitja Institute |
| Leila Smith | Lowitja Institute |
| Mark Glazebrooke | Lowitja Institute |
| Paulene Mackell | National Ageing Research Institute |
| Alan Singh | NHMRC |
| Anne Kelso | NHMRC |
| Wee-Ming Boon | NHMRC |
| Sam Faulkner | NHMRC |
| Tony Kingdon | NHMRC |
| Zoe Kelly | NHMRC |
| Dan McAullay | PCIC, NHMRC |
| Sandra Eades | PCIC, NHMRC |
| Yvette Roe | PCIC, NHMRC |
| Dina LoGiudice | University of Melbourne |
| Louise Lyons | Victorian Aboriginal Community Controlled Health Organisation |
| Deborah Zion | Victoria University |
| Name | Organisation |
|---|---|
| James Harris | Aboriginal Health Council of Western Australia |
| Rob McPhee | Aboriginal Health Council of Western Australia |
| Tara Rowe | Aboriginal Health Council of Western Australia |
| Ben Horgan | Consumer and Community Health Research Network |
| Alisa Munns | Curtin University |
| Cheryl Davis | Curtin University |
| Nikayla Crisp | Curtin University |
| Paul Bell | Koorliny Moort Program |
| Alan Singh | NHMRC |
| Sam Faulkner | NHMRC |
| Tony Kingdon | NHMRC |
| Dan McAullay | PCIC, NHMRC |
| Yvette Roe | PCIC, NHMRC |
| Brad Farrant | Telethon Kids Institute |
| Carol Michie | Telethon Kids Institute |
| Glenn Pearson | Telethon Kids Institute |
| Isabelle Adams | Telethon Kids Institute |
| Mara West | Telethon Kids Institute |
| Michael Wright | Telethon Kids Institute |
| Jonathan Carapetis | Telethon Kids Institute |
| Roz Walker | Telethon Kids Institute |
| Julia Marley | The Rural Clinical School of Western Australia |
| Shane Hearn | University of Adelaide |
| Kate Smith | University of Western Australia |
| Kimberley McAuley | University of Western Australia |
| Natalie Strobel | University of Western Australia |
| Lenny Papertalk | University of Western Australia |
| Lianne Gilchrist | University of Western Australia |
| Leon Flicker | University of Western Australia |
| Judy Katzenellenbogen | University of Western Australia |
| Marilyn Lyford | Western Australian Centre for Rural Health |
| Michele Holloway | Western Australian Centre for Rural Health |
| Sandra Thompson | Western Australian Centre for Rural Health |
| Name | Organisation |
|---|---|
| Elizabeth Luland | Aboriginal Health & Medical Research Council of NSW |
| Margaret Cashman | Aboriginal Health & Medical Research Council of NSW |
| Leo Carroll | Australian Institute of Health and Welfare |
| Colleen Gibbs | The Congress of Aboriginal and Torres Strait Islander Nurses and Midwives |
| Jessica Stewart | Department of Family and Community Services |
| Karl Briscoe | National Aboriginal and Torres Strait Islander Health Worker Association |
| Alan Singh | NHMRC |
| Naomi Gowor | NHMRC |
| Sam Faulkner | NHMRC |
| Tony Kingdon | NHMRC |
| Dan McAullay | PCIC, NHMRC |
| Sandra Eades | PCIC, NHMRC |
| Christina (Tina) Hourigan | Tresillian |
| Marlene Kong | University of New South Wales |
| Telphia-Leanne Joseph | University of New South Wales |
| Vanessa Lee | University of Sydney |
| Name | Organisation |
|---|---|
| Karla Canuto | Apunipima |
| Scott Ritchie | Australian Institute of Tropical Health & Medicine, James Cook University |
| Andrew Johnson | Australian Institute of Tropical Health and Medicine |
| Louis Schofield | Australian Institute of Tropical Health and Medicine |
| Maxine Whittaker | James Cook University |
| Robyn McDermott | James Cook University |
| Emma McBryde | James Cook University |
| Ian Wronski | James Cook University |
| Alan Ramsay | James Cook University |
| Kate McConnon | Medical Services, Torres and Cape Hospital and Health Service |
| Rosemary Schmidt | Medical Services, Torres and Cape Hospital and Health Service |
| Sam Faulkner | NHMRC |
| Tony Kingdon | NHMRC |
| Ali Drummond | PCIC, NHMRC |
| Andrea Mann | QLD Health |
| Andrew Berry | QLD Health |
| Jennifer Wharton | QLD Health |
| Betty Sagigi | QLD Health |
| Maria Tapim | QLD Health |
| Yancy Laifoo | QLD Health |
| Sean Taylor | QLD Health |
| Aggie Hankin | QLD Health |
| Venessa Curnow | QLD Health |
| Alexandra Hofer | Thursday Island Hospital |
| Kerry Dixon | Torres Strait Regional Authority |
| Chelsea Aniba | Torres Strait Regional Authority |


