While Australia now has one of the lowest tuberculosis (TB) incidence rates in the world, TB was once a leading cause of death in Australia and was a focus for public health policy during the first half of the 20th century.
NHMRC, and its precursor the Federal Health Council, were active participants in broader government efforts to prevent and control the spread of TB. These efforts were underpinned by research, and research projects related to TB were some of the earliest that NHMRC funded. This case study focuses on the role played by NHMRC and Australian governments in the virtual eradication of TB in Australia during the 20th century.
A landscape format version of this case study is available as a PDF from the Downloads section below.
Origin
TB is a contagious bacterial disease spread through the air that especially affects the lungs. It causes fever-like symptoms, destruction of tissue and often death if not treated.
People living in poor housing and environmental conditions, who have lower food security and less access to quality health care, are at greater risk of both contracting and dying from this disease.
At the beginning of the 20th century, TB was a major cause of death in Australia – ranking first among females and second among males.
In 1925 a Federal Royal Commission on Health recommended that the recently established Commonwealth Department of Health should formulate a plan for a campaign against the spread of TB. It also recommended the formation of a Federal Health Council to provide advice to government. The council was established in 1927 along with a Division of Tuberculosis within the Department of Health.
At its first meeting, the council set about the task of developing a national campaign against TB and in 1929 it adopted a report by Dr Mervyn Holmes, the first Director of Tuberculosis, laying out a plan for the control of TB in Australia. However, implementation of this plan was delayed by the economic depression of the 1930s.
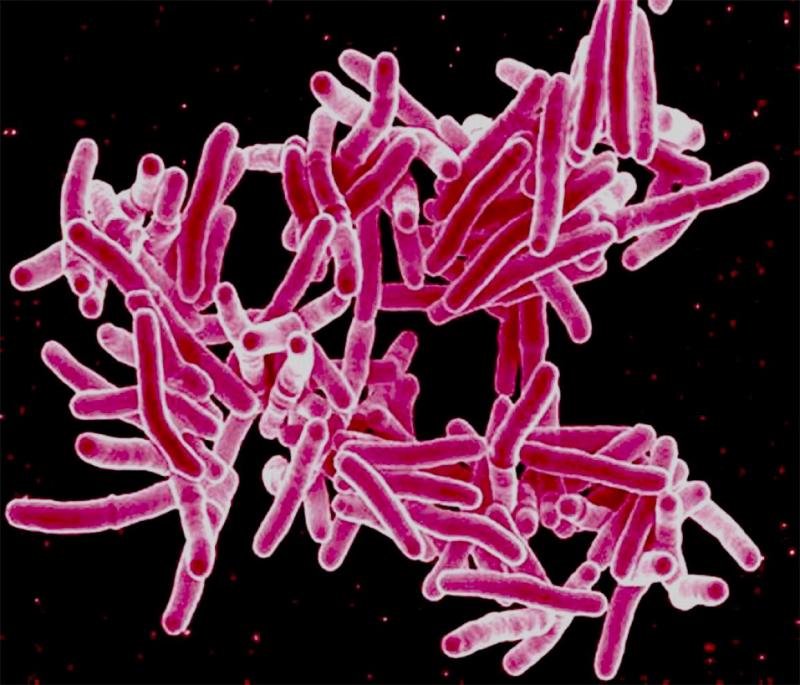
Credit: National Institute of Allergy and Infectious Disease
Mycobacterium tuberculosis, the bacterium which causes TB.
Research and Investment
In 1936 the Federal Health Council was increased in size, its powers were expanded to include research and it was renamed as the National Health and Medical Research Council (NHMRC). In 1937, during its third session, the council established a Standing Committee on Tuberculosis. The committee began its work by collating available statistics on TB infection rates. This was the first effective and nationally coordinated effort to map the incidence of TB in Australia.
NHMRC, based upon recommendations made by the committee, also began directly funding research into TB. Early grants for TB-related research included: a study in Frankston, Victoria, of children with TB of bones and joints; a Sydney-based study of TB infection in children, adolescents and young adults; and an investigation of TB in childhood and the relationship between human and bovine infection.
The fourth council session approved a grant to Dr Harry Wunderly who performed experiments using micro-radiography for TB detection and suggested that this approach would be suitable for use in large surveys. NHMRC directed the Commonwealth X-ray and Radium Laboratory to undertake this work and by 1942 Dr Cecil Eddy from the laboratory had devised an apparatus to conduct the mass screening of TB.
In 1945, Dr Nancy Atkinson, a bacteriologist at the Institute of Medical and Veterinary Science in Adelaide, produced the first Australian made Bacillus Calmette-Guérin (BCG) vaccine against TB. This vaccine was later produced in quantity by the Commonwealth Serum Laboratories (CSL). NHMRC funded Dr Atkinson’s bacteriological research from 1944 to 1952, including her work on BCG.
Advice
Some of NHMRC’s earliest advice to government concerned the importance of increasing financial support for those infected with TB in order to allow them to take time away from their families and workplaces. In 1939 the Federal Government responded to this advice by making an adjustment to its invalid pension policy allowing TB sufferers to become eligible for the invalid pension while in early stages of the disease.
In 1941 the Minister for Health requested NHMRC’s advice on the best method of ‘attacking’ TB. NHMRC recommended implementation of a mass screening program that could be commenced “as soon after the conclusion of the war as facilities become available”. By 1942, Eddy’s microradiography apparatus had been adopted for the routine examination of all entrants to the armed services.
In 1942 NHMRC was asked by the Joint Parliamentary Committee on Social Security (JPCSS) to provide advice on a possible program on TB – amongst other health issues – that could be implemented during the war. NHMRC’s response included outlining how a mass screening program could work and how much it would cost, informed by the results of Wunderly’s research.
Informed by NHMRC’s work, a 1943 conference of Ministers for Health agreed that a national campaign for the early detection and treatment of TB should be planned in all states and that NHMRC’s state representatives should outline a scheme that could then be funded by the Commonwealth.
In 1943 the JPCSS provided Parliament with recommendations for a national campaign against TB based upon this work
Implementation
The Australian Parliament passed the Tuberculosis Act 1945 based on recommendations from the JPCSS. The Act created the first comprehensive national health campaign to eradicate TB. However, there were constitutional problems surrounding the Commonwealth’s involvement in the TB campaign which had to be addressed through a 1946 referendum that passed social services power to the Commonwealth.
A new Act, the Tuberculosis Act 1948, permitted the Commonwealth to lead national efforts to control TB. The plan set out in this Act was informed by a report by Wunderly, who had been appointed Director of Tuberculosis. To implement the resultant Australian Tuberculosis Campaign (ATC), a council of medical experts was formed. This National Tuberculosis Advisory Council (NTAC) first met in September 1949.
The ATC ran from 1948 to 1976, providing citizens with free diagnostic chest X-rays, medical care and a Tuberculosis Allowance while being treated. Where X-rays detected an abnormality, this would lead to further testing in hospital and subsequent treatment.
The introduction of antibiotics such as streptomycin and isoniazid in 1945 and 1952 respectively had a significant impact on the reduction of TB rates. These were provided free of charge by the ATC to all diagnosed cases.
The ATC was ceased in 1976 following marked decreases in the prevalence of TB. However, NTAC remains in existence to provide national advice on TB prevention and control.
Outcomes and Impact
The age-standardised death rate from TB in Australia dropped dramatically during the 20th century, from 108.5 per 100,000 population in 1907 to 0.3 per 100,000 population in 2000.
This decline in incidence can be attributed to various improvements over the century including improved general standards of nutrition, housing and sanitation, and improved medical and hospital services.
In 2007 the incidence rate of TB in Australia was 5.4 cases per 100,000, one of the lowest rates in the world. However the absolute numbers of TB cases increased by 33% between 1998 and 2008, corresponding with Australia’s migration intake and increasing population.
NHMRC continues to support research focused on TB, with over $63 million in grants provided from 2009 to 2018.

Source: ABS GRIM Book Version 9 2008
Timeline
| Date | Event |
|---|---|
| 1921 | Federal Health Department established |
| 1925 | Federal Royal Commission on Health |
| 1927 | Federal Health Council established |
| 1936 | NHMRC established |
| 1938 | NHMRC Grants |
| 1939 | Invalid pension for TB sufferers |
| 1939 | NHMRC Grants |
| 1941 | NHMRC Grants |
| 1943 | NHMRC Grant |
| 1943 | Recommendations to Parliament on TB campaign |
| 1944 | NHMRC Grant |
| 1945 | Atkinson produces first TB vaccine in Australia |
| 1945 | Tuberculosis Act 1945 |
| 1947 | NHMRC Grants – incl. Atkinson for BCG |
| 1948 | Tuberculosis Act 1948 |
| 1948 | NHMRC Grants – incl. Atkinson for BCG |
| 1949 | NTAC established |
| 1949 | NHMRC Grants |
Researcher profiles
Sir Harry Wyatt Wunderly
Harry Wunderly (1892-1971) was a medical practitioner and public health administrator. He was a lieutenant colonel in the Australian Army Medical Corps and was Director of Tuberculosis in the Commonwealth Department of Health. He was a fellow of the Royal Australian College of Physicians and the Royal College of Physicians (London) and President of the National Association for the Prevention of Tuberculosis in Australia. He was also a consultant for the World Health Organisation.
Dr Cecil Ernest Eddy
Cecil Eddy (1900-1956) was a radiological physicist. He received a Rockefeller Foundation fellowship to work under Sir Ernest Rutherford at the Cavendish Laboratory, Cambridge, England. He was chair of the NHMRC standing committees on X-rays and radioactive isotopes and also chair of the United Nations scientific committee on the effects of atomic radiation.
Dr Nancy Atkinson DSc OBE
Nancy Atkinson (1910-1999), an Australian bacteriologist, was the first person to produce penicillin in Australia. In the 1950s, as a researcher at the Institute of Medical and Veterinary Science in Adelaide, she undertook research focused on antibiotics, salmonellas and other groups of bacteria, and vaccines for tuberculosis and typhoid. In 1951 she was appointed to the Order of the British Empire (OBE) and recognised as one of the world’s leading authorities on bacteriology.
Dr John H L Cumpston CMG
John Cumpston (1880-1954) was a public health administrator. He received his medical training in Melbourne and a Diploma in Public Health in London. In 1921 he became the first Director-General of the Australian Government Department of Health and later, in that same capacity, the Chair of the Federal Health Council (1927-1936) and of NHMRC (1937-1945). In 1929 he was made Companion of The Most Distinguished Order of St. Michael & St. George, for his services to the Commonwealth.
Dr Mervyn John Holmes
Mervyn Holmes (1884-1965) was appointed the first Commonwealth Director of Tuberculosis in 1925 and was responsible for the TB and radium clinics at Canberra Hospital as Medical Officer of Health for the Territory. After enlisting he was posted as Director of Army Hygiene, Victoria Barracks, Melbourne, and was attached to General Douglas Macarthur's headquarters in Brisbane from 1943 to 1945, serving on the Combined Advisory Committee on Tropical Medicine, Hygiene & Sanitation. He was a member of the Federal Health Council and then of NHMRC from 1927 to 1944.
References
In developing this case study, extensive use was made of NHMRC’s internal database of Council Session reports.
Other reference sources consulted include:
Australian Institute of Health and Welfare. (2005). Mortality over the twentieth century in Australia: Trends and patterns in major causes of death. Mortality Surveillance Series, 4(PHE73). AIHW.
Australian Institute of Health and Welfare. (2008). Tuberculosis (including late effects). General Record of Incidence of Mortality (GRIM) Books Version 9. ICD10 A15-A19, B90. AIHW.
Craven, B. (2010). Shoulders of Giants: Achievements in History’s War on Tuberculosis. Blue Mountains Historical Society Inc.
Didn’t know of her O.B.E. News (Adelaide, SA: 1923-1954), 1 January 1951, p 1. National Library of Australia. https://trove.nla.gov.au/newspaper/article/130366288 [Accessed 3 April 2020)
Lonie, C., Levy, M., and Frommer, M. (1994). Counting the costs: A review of two tuberculosis mass contact screening investigations. New South Wales Public Health Bulletin, 5(2). NSW Government.
McEwin, E. (2018). Nancy Atkinson, bacteriologist, winemaker and writer. Australian Journal of Biography and History. 2018(1), pp 59-77. ANU Press. doi.org/10.22459/AJBH.2018.03
National Tuberculosis Advisory Committee. (2012). The strategic plan for control of tuberculosis in Australia: 2011-2015. Communicable Diseases Intelligence, 36(3). Australian Government Department of Health.
Oxlade, O. and Murray, M. (2012). Tuberculosis and Poverty: Why Are the Poor at Greater Risk in India? PLoS ONE, 7(11), doi:10.1371/journal.pone.0047533
Putland, C. (2012). Tuberculosis and the Australian state: Australia’s National Anti-tuberculosis Campaign 1898-1948. An Administrative History of a Public Health Policy. A thesis submitted for the degree of Doctor of Philosophy in the Department of History School of International Studies, Flinders University. Adelaide, South Australia.
Robertus, L., Konstantinos, A., Hayman, N. and Paterson, D. (2011). Tuberculosis in the Australian Indigenous population: history, current situation and future challenges. Australian and New Zealand Journal of Public Health. 35(1), pp 6-9.
Stylianou, M. (2009). ‘A Scandal Which Must be Corrected’: Reconsidering the Success of the Australian Tuberculosis Campaign. Health History, 11(2), pp. 21-41.
Toms, C. Stapledon, R., Coulter, C., Douglas, P. and the National Tuberculosis Advisory Committee. (2014). Tuberculosis notifications in Australia, 2014. Communicable Diseases Network Australia and the Australian Mycobacterium Reference Laboratory Network. Australian Government Department of Health.