Worldwide, preterm birth (birth before 37 weeks) is the single largest cause of death in the newborn period and early childhood.1 In Australia each year, around 8% of babies (almost 26,000 in 2019)2 are born prematurely. A wide variety of health issues are associated with pre-term birth, including developmental delay, cerebral palsy, hearing and visual impairments, learning difficulties and psychiatric disorders. NHMRC-funded researchers at the South Australian Health and Medical Research Institute (SAHMRI) and other Adelaide-based institutions have made major contributions to reducing the prevalence of premature births and improving the health of premature babies.
- Video transcript
0:07
My name is Maria Makrides, and I'm the Theme Leader for SAHMRI Women and Kids, based at the South Australian Health and Medical Research Institute in Adelaide.I started my research life as a dietitian after having done a science degree at the University of Melbourne and then Bachelor of Nutrition and Dietetics at Flinders University here in Adelaide. I worked out pretty quickly that I wanted to work more in research rather than being a clinical dietitian.
0:41
So I took the opportunity to do a PhD in paediatric nutrition and was involved in some of the first studies to work out the omega-3 requirements for term babies.I've continued to work in the field of omega-3 fatty acids probably for the last 25 years or so. So it has been a long journey, and the field has evolved a lot during that time.
We've gone from not really understanding the role of omega-3 fatty acids may play, to supporting the healthy development of babies, both those born at term as well as those that are born early.1:26
Some of the earliest work that I was involved with as part of my PhD and led was doing the very first supplementation studies of adding these omega-3 fatty acids to infant formulas.The reason why we thought that that may have been important is that in the early 90s, there were many studies showing a lot of developmental differences between babies that were fed infant formulas compared to those who were breastfed at that time.
Most infant formulas or all infant formulas did not have added omega-3 fatty acids, whereas breast milk had a full spectrum of all omega-3 fatty acids.
2:10
In fact, most infant formulas had a preponderance of the omega-3 fatty acids and even very few of the precursor fatty acids.So the very early studies were really doing supplementation studies, and what we managed to show is that when omega-3s are added to those early style of infant formulas, that we were able to improve the visual development of babies who were formula fed and otherwise had no omega-3 fatty acids in their diet.
Obviously, the field has evolved hugely since then, and the quality of the infant formulas has changed. But a lot of the more recent work has been about how do we support the development of those babies that are born very early.
3:04
And these babies that are born so early miss the last trimester of pregnancy, which is a time that these omega-3 fatty acids are accumulated into the brain when it has its brain growth spurt.And this particular fatty acid called DHA, makes up about a third of all the lipid in the brain, so is thought to have quite an important role.
So the field has evolved to be more than just thinking about infant formula and breast milk and looking at the requirements. So the babies that are born very early, we think have requirements that are above what is currently in the diet either from the mother's expressed breast milk or the supplemented formula.
So we have developed and tested an emulsion that can be added to whatever the baby is fed to try and meet what it would have if it was still in the womb.
4:07
And what we've managed to show is that for the very preterm babies, by meeting that in utero requirement we can improve the development of those babies and improve their IQ out at 5 years of age.The impact of the work, particularly the trials that we've done here in Adelaide, as well as many other people around the world, has been to legislate changes in the composition of infant formulas so that there are minimum levels. For the precursor omega-3 fatty acid called alpha linolenic acid and also allowing the optional addition of the longer chain omega-3 fatty acids for term babies as well as for preterm babies.
4:55
So those legislative changes have been made in over 180 countries around the world.Well, what drives the passion in the work is really about building from making sure that there's a strong foundation and then building on that and the next step and the next step to really try and make solid change for the long-term health of children and babies everywhere outside of work.
As a nutritionist I love having dinner parties and I love sitting around with friends and colleagues over a table and sharing a lovely meal. I love long beach walks and really walking out in nature.
End of transcript.
Origin
As far back as 1927, the Federal Health Council (NHMRC’s precursor) received a report that the mortality rate for the first month of life was about 30 deaths per 1,000 births, and the report noted that these deaths were mostly due to prematurity and congenital causes connected with conditions arising before or during birth.3 Subsequent reports highlighted that the mortality of premature infants could be lowered substantially with improved maternal diet.4
By 1981, NHMRC had issued statements about diet in pregnancy, lactation and early infant feeding, and in that year the first National Nutrition Education Conference was held, following a recommendation by NHMRC. The conference recommended that those providing direct care to pregnant and lactating women should be given sufficient and scientifically up-to-date information to enable those women to make food choices to meet the nutrient requirements of pregnancy and lactation.5
Also in 1981, and at Flinders Medical Centre in South Australia, Robert Gibson published pioneering research on the fatty acid composition of human colostrum (the first milk produced by breasts) in comparison to mature breast milk. The research found, among other things, that colostrum includes a higher percentage long-chain polyunsaturated fatty acids, including the four types of omega-3 fatty acids.
Investment
After Maria Makrides completed a post graduate degree in nutrition and dietetics at Flinders University (1991), she commenced a PhD in paediatric nutrition in 1992, supervised by Gibson. Commencing in 1994, the work of Makrides, Gibson and a group of colleagues at Flinders, the Women’s and Children’s Hospital, University of Adelaide and SAHMRI, was supported by a succession of NHMRC grants.
The work described in this case study was also supported by:
- The Channel 7 Children’s Research Foundation
- The Women’s and Children’s Hospital Foundation
- Thyne Reid Foundation
- The Hospital Research Foundation Group
- Medical Research Future Fund
- National and international industry partners including Clover Corporation, Efamol, Nestle, Wyeth Nutritionals, and Mead Johnson Nutritionals.
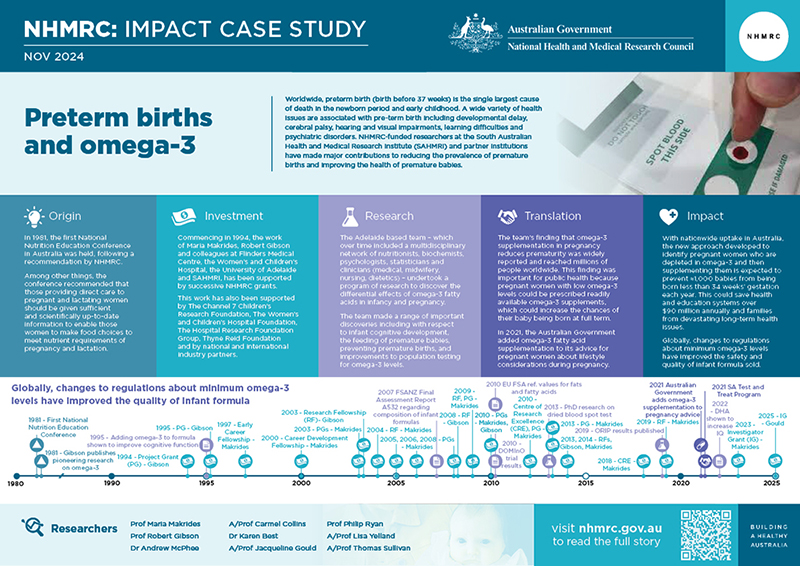
The PDF poster version of this case study includes a graphical timeline showing NHMRC grants provided and other events described in the case study.
Research
The Adelaide-based team – which over time comprised a multidisciplinary network of collaborators including nutritionists, biochemists, psychologists, biostatisticians and clinicians (medical, midwifery, nursing, dietetics) – undertook a program of research to discover the differential effects of omega-3 fatty acids in infancy and pregnancy, and made a range of important discoveries.
Cognitive development
When the team’s research began, infant formula usually contained only minute levels of omega-3 fatty acids that are essential components of brains. The team discovered – and this finding was soon reproduced by others overseas – that delayed visual and neural maturation of term infants fed these formulas could be improved to be at the same levels as those of breastfed infants, by adding omega-3s to infant formula.6
Feeding premature infants
One type of omega-3, called DHA, makes up about one third of lipid (fats) in the brain. Very preterm infants have DHA requirements above what they can get from breast milk or formula because babies who remain in utero receive more DHA. The team conducted two large randomised trials: the first with 657 babies born more than 9 weeks premature;7 and the second larger study, with 1273 babies born at least 11 weeks premature.8 The team found that by meeting a very preterm infant’s in utero requirements for DHA, the infant’s IQ at 5 years would be closer to what would be expected if it had not been born preterm.9
Preventing premature births
In the 1980s, reports from the Faroe Islands highlighted that the high consumption of fish rich in omega-3 fats was associated with longer gestation and higher average birthweight of liveborn singleton infants. This was followed in 1992 by a randomised trial of over 500 women that showed that fish oil extended the duration of pregnancy in Danish women. The hypothesis proposed was that dietary omega-3 in high amounts prolonged gestation in human beings by interfering with uterine production of prostaglandins which are mediators of uterine contractions and cervical ripening. Although it was suggested as a possibility, there was no strong direct evidence that omega-3 fatty acids could prevent premature birth.
Makrides and Gibson’s DOMInO trial involving 2399 pregnant women tested the effect of 800 mg of DHA per day compared with a vegetable oil mix. Secondary analyses showed that there was a halving of early preterm birth rates.10 This gave the group the pilot data to gain NHMRC funding and mount their largest and most definitive trial (called ORIP) that involved over 5500 women.11 It took two years of exhaustive analyses to determine the full extent of the effects of DHA. It turns out that DHA was mainly effective in women who had low omega-3 levels in their blood and only if they were carrying one baby (singleton women).12 This turned out to be around 20% of all pregnant women.
Minimally invasive technique
In all their early trials, the team was hampered by the cost and complexity of the procedures necessary to measure omega-3 fatty acids in blood samples. To simplify the process of testing omega-3 levels, the team developed and validated a dried blood spot test that allowed the delivery of blood samples from enrolling centres around Australia, New Zealand and Singapore to their central laboratory in Adelaide. Importantly, the blood collection cards enabled the cards to be stored without refrigeration and could be transported by the postal system. It also allowed the group to screen a range of metabolic derivatives of DHA that gave clues to the mechanism of action of DHA in pregnancy.

Translation
The SAHMRI team’s finding that supplementation in pregnancy reduces prematurity was widely reported in the media and this information reached millions of people worldwide. This finding was important for public health because pregnant women with low omega-3 levels could be prescribed readily available omega-3 supplements, which could increase the chances of their baby being born at full term.
In 2021, the Australian Government added omega-3 fatty acid supplementation to its advice for pregnant women about lifestyle considerations during pregnancy. Similar evidence-based recommendations have since been made by other international guidelines.13, 14, 15
Also in 2021, and in partnership with SA Pathology, the SAHMRI team developed the community Omega-3 Test-and-Treat Program. Since its establishment, the program has provided free omega-3 screening to over 22,000 women in South Australia, with over 800 pregnant women being tested each month. About 17% of women tested are found to have low omega-3 levels and are advised about specific supplementation.
The team’s perinatal nutrition program led to advances in prenatal care to prevent early birth to reduce risk of death and disability in babies, as well as changes in international food laws for infant foods. These legislative changes have been made in the EU as well as 180 countries globally.
Outcomes and impacts
The new approach developed by the SAHMRI team, to identify pregnant women who are depleted in omega-3 and then supplementing them, is expected to prevent ≈1,000 babies from being born less than 34 weeks’ gestation each year with nation-wide uptake (in Australia), potentially saving health and education systems over $90 million annually and families from devastating long-term health issues.
In Australia, preterm birth, especially early preterm birth, accounts for more than 85% of all perinatal complications and neonatal deaths and can have life-long consequences. Prematurity represents a significant psychological and financial toll on parents and a substantial societal economic burden, estimated to cost $1.6 – $2.6 billion annually in Australia.16
Globally, an estimated 13.4 million babies were born preterm in 2020 and preterm birth complications are the leading cause of death among children under 5 years of age, responsible for approximately 900,000 deaths in 2019.17, 18
Before the SAHMRI team commenced its research, infant formulas contained little or no omega-3. Now, and globally, changes to regulations about minimum omega-3 levels for infant formula have improved the safety and quality of over 2.7 million tonnes of infant formula sold each year.
Optimising omega-3 nutrition for the tiniest babies has the potential to improve cognitive abilities and support their long-term productivity. It is estimated that each IQ point raises worker productivity by 1.8% to 2.4%, resulting in substantial economic benefit in lifetime earnings and societal contribution.
Global suppliers are now marketing omega-3 testing kits, and omega-3 screen-and-treat programs for pregnant women are available in the UK and USA.
Researchers
Professor Maria Makrides
Maria Makrides completed a Bachelor of Science (University of Melbourne 1989) and a post graduate degree in Nutrition and Dietetics (Flinders University 1991), followed by a PhD in paediatric nutrition in 1995 (Flinders University). She is currently Executive Director of SAHMRI. Maria is an elected Fellow, and only dietitian, of the Australian Academy of Science (2019), Fellow of the Australian Academy of Health and Medical Science (2014) and Fellow of the Nutrition Society of Australia (2012). She received the Alexander Leaf Distinguished Scientist Award for Lifetime Achievement from the International Society for the Study of Fatty Acids and Lipids (ISSFAL) in 2018 and served as President from 2021 to 2024. Maria was awarded South Australian Scientist of the Year in 2022.
Professor Robert A Gibson
Robert Gibson completed his PhD at the University of Adelaide in 1975. He was previously the Director of the FOODplus Research Centre at The University of Adelaide and is currently Emeritus Professor, School of Agriculture, Food and Wine, University of Adelaide. Robert was awarded the 2003 Nutrition Society of Australia, Research Medal and in 2004 was made a Fellow, Nutrition Society of Australia. In 2012 he was awarded the Alexander Leaf Distinguished Scientist Award for Lifetime Achievement and in 2016 made a Fellow of the International Society for the Study of Fatty Acids and Lipids (ISSFAL).
Dr Andrew McPhee
Andrew McPhee studied Medicine at the University of Adelaide, graduating in 1976 (MBBS). After undertaking registrarships at Adelaide Children's Hospital, Flinders Medical Centre, Queen Victoria Hospital, and Alice Springs Hospital he received his Fellowship of the Australasian College of Physicians (FRACP, Paediatrics) in 1982. He then completed fellowship training in Neonatology at University of Cincinnati, Children's Hospital Medical Center (Cincinnati, Ohio) and The Queen Victoria Hospital (1982-1985). Andrew was Director of the Neonatal ICU, Queen Victoria Hospital / Women’s and Children’s Hospital from 1993-2012, State Director of Neonatal Medicine through 2013-2018, and served as Chair of the Advanced Training Committee in Neonatal- Perinatal Medicine of the RACP (2014-2016).
Associate Professor Carmel Collins
Carmel Collins (1959-2024) began her career as a Registered Nurse completing her General Nursing degree at the Mt Gambier School of Nursing and Midwifery (1980) and then a Midwifery degree at the Bangour College of Nursing and Midwifery in Scotland (1983). She then completed a PhD in public health at The University of Adelaide in 2004. She was previously the Head of the Neonatal Nutrition Research Unit at SAHMRI. Carmel received the New Investigator Award from the Perinatal Society of Australia and New Zealand (PSANZ) in 2001, was awarded a Life Member of the Australian College of Neonatal Nurses in 2002 and was the winner of the South Australian Nursing Excellence Award in 2009.
Dr Karen Best
Karen Best received a Registered Nursing Certificate from the Queen Elizabeth Hospital, Adelaide, South Australia, in 1987, followed by a Registered Midwifery Certificate from the Queen Victoria Hospital, Adelaide, in 1991. After several years of clinical practice at the Women’s and Children’s Hospital, in 2005 she completed a Post-graduate Advanced Certificate in Clinical Trials Management from the University of Canberra. Awarded the MS McLeod Paediatric and Child Health Nursing PhD Scholarship in 2012, Karen earned her PhD in Paediatrics at the University of Adelaide under the supervision of Professor Makrides. She joined Maria's team as a Postdoctoral Fellow and led the ‘Omega-3 to Reduce the Incidence of Preterm Birth’ (ORIP) Trial and other perinatal projects, and in 2020, was awarded the MS McLeod Post-doctoral Research Fellowship. From 2022 to 2024, Karen served as Director of SAHMRI’s Clinical Trials Platform. She now serves as Co-lead of the Pregnancy & Newborn Health Research Program within SAHMRI’s Women and Kids Theme.
Associate Professor Jacqueline Gould
Jacqueline Gould graduated with a Bachelor of Social Science and a Bachelor of Health Science (Honours) from the University of Adelaide in 2008. She completed her PhD in Paediatrics in 2013 at the University of Adelaide under the supervision of Professor Makrides and Professor Gibson. She held postdoctoral positions at the Women’s and Children’s Health Research Institute (2013-2016) and SAHMRI (2016 onwards). Jacqueline received a MS McLeod Postdoctoral Research Fellowship (2016-2018), the Dr Norman Salem Jnr International Early Career Award (2023). She became Associate Professor in 2024, and leads the Supporting Neurodevelopment Program at SAHMRI Women and Kids.
Professor Philip Ryan
Philip Ryan completed his Bachelor of Medicine and Bachelor of Surgery at the University of Sydney in 1977. He then went on to complete his Bachelor of Science at the Australian National University in 1984. He was previously the Director of the Data Management and Analysis Centre (DMAC) at The University of Adelaide and currently holds Emeritus Professor status at The University of Adelaide. Philip was made a Fellow of the Faculty of Public Health Medicine by the Royal Australasian College of Physicians (RACP) in 1991 and received the Basil S Hetzel Award for Public Health Leadership (PHAA) in 2013.
Associate Professor Lisa Yelland
Lisa Yelland graduated with a Bachelor of Mathematical and Computer Sciences (first class honours in statistics) from The University of Adelaide in 2004. After several years of working as a biostatistician on trials including DOMInO, she undertook a PhD in statistical methods for randomised trials at The University of Adelaide, which she completed in 2011. She then held post-doctoral positions at The University of Adelaide (2011-2020) and SAHMRI (2020-present), during which time she was lead statistician for the ORIP trial. She is currently Co-Leader of both the Perinatal Trial Methodology Program within the SAHMRI Women and Kids Theme, and the SAHMRI Biostatistics Unit.
Associate Professor Thomas Sullivan
Thomas Sullivan graduated with a Bachelor of Social Sciences (2003) and a Bachelor of Mathematical and Computer Sciences (first class honours in statistics, 2005) from The University of Adelaide. From 2005-14 he worked as a consulting statistician at The University of Adelaide, taking on lead statistician roles on several clinical trials, including N3RO and DINO. He then undertook a PhD and Masters of Biostatistics at The University of Adelaide, completing these programs in 2017 and 2018, respectively. He has since held a post-doctoral position at SAHMRI and is currently Co-Leader of the Perinatal Trial Methodology Program within the SAHMRI Women and Kids Theme.
Partners
This case study was developed with input from Professor Maria Makrides and Professor Robert Gibson and in partnership with SAHMRI.
References
The information and images from which impact case studies are produced may be obtained from a number of sources including our case study partner, NHMRC’s internal records and publicly available materials. Key sources of information consulted for this case study include:
1 Chang HH, Larson J, Blencowe H et al. Preventing preterm births: analysis of trends and potential reductions with interventions in 39 countries with very high human development index. Lancet 2013; 381: 223–234.
2 Qiao C, Menon R, Ahn KH, Suzuki S, Kshetrapal P, Georgiou HM, Mesiano S, Zhong N. Preterm birth update in Australasia: A report of the international symposium of Preterm Birth International Collaborative-Australasia branch. Frontiers in Pediatrics. 2022 Jul 25;10:903546.
3 Federal Health Council. Report of the Federal Heath Council of Australia: First Session held at Melbourne, 25-28th January 1927. Commonwealth of Australia, Melbourne 1927. p185
4 National Health and Medical Research Council. Report of the NHMRC Council Session: Twenty-Sixth Session held at Sydney NSW, 17th and 18th November, 1948. Commonwealth of Australia, Canberra, 1948. p115.
5 National Health and Medical Research Council. Commonwealth Department of Health, Report of the ninety-second session, Canberra, October 1981. Australian Government Publishing Service, Canberra 1982. p745
6 Makrides M, Neumann M, Simmer K, Gibson R, Pater J. Are long-chain polyunsaturated fatty acids essential nutrients in infancy?. The Lancet. 1995 Jun 10;345(8963):1463-8.
7 Makrides M, Gibson RA, McPhee AJ, Collins CT, Davis PG, Doyle LW, Simmer K, Colditz PB, Morris S, Smithers LG, Willson K. Neurodevelopmental outcomes of preterm infants fed high-dose docosahexaenoic acid: a randomized controlled trial. Jama. 2009 Jan 14;301(2):175-82.
8 Collins CT, Makrides M, McPhee AJ, Sullivan TR, Davis PG, Thio M, Simmer K, Rajadurai VS, Travadi J, Berry MJ, Liley HG. Docosahexaenoic acid and bronchopulmonary dysplasia in preterm infants. New England Journal of Medicine. 2017 Mar 30;376(13):1245-55.
9 Gould JF, Makrides M, Gibson RA, Sullivan TR, McPhee AJ, Anderson PJ, Best KP, Sharp M, Cheong JL, Opie GF, Travadi J. Neonatal docosahexaenoic acid in preterm infants and intelligence at 5 years. New England Journal of Medicine. 2022 Oct 27;387(17):1579-88.
10 Makrides M, Gibson RA, McPhee AJ, Yelland L, Quinlivan J, Ryan P, DOMInO Investigative Team AT. Effect of DHA supplementation during pregnancy on maternal depression and neurodevelopment of young children: a randomized controlled trial. Jama. 2010 Oct 20;304(15):1675-83.
11 Makrides M, Best K, Yelland L, McPhee A, Zhou S, Quinlivan J, Dodd J, Atkinson E, Safa H, Van Dam J, Khot N. A randomized trial of prenatal n− 3 fatty acid supplementation and preterm delivery. New England Journal of Medicine. 2019 Sep 12;381(11):1035-45.
12 Simmonds LA, Sullivan TR, Skubisz M, Middleton PF, Best KP, Yelland LN, Quinlivan J, Zhou SJ, Liu G, McPhee AJ, Gibson RA. Omega‐3 fatty acid supplementation in pregnancy—baseline omega‐3 status and early preterm birth: exploratory analysis of a randomised controlled trial. BJOG: An International Journal of Obstetrics & Gynaecology. 2020 Jul;127(8):975-81.
13 Best KP, Gibson RA, Makrides M. ISSFAL statement number 7 - Omega-3 fatty acids during pregnancy to reduce preterm birth. Prostaglandins Leukot Essent Fatty Acids. 2022;186:102495.10.1016/j.plefa.2022.102495
14 Cetin I, Carlson SE, Burden C, et al. Omega-3 fatty acid supply in pregnancy for risk reduction of preterm and early preterm birth. Am J Obstet Gynecol MFM. 2024;6(2):101251.10.1016/j.ajogmf.2023.101251
15 Savona-Ventura C, Mahmood T, Mukhopadhyay S, et al. Omega-3 fatty acid supply in pregnancy for risk reduction of preterm and early preterm birth: A position statement by the European Board and College of Obstetrics and Gynaecology (EBCOG). Eur J Obstet Gynecol Reprod Biol. 2024;295:124-5.10.1016/j.ejogrb.2024.02.009
16 Newnham JP, Schilling C, Petrou S, et al. The health and educational costs of preterm birth to 18 years of age in Australia. Aust N Z J Obstet Gynaecol. 2022;62:55-61
17 Ohuma E, Moller A-B, Bradley E, et al. National, regional, and worldwide estimates of preterm birth in 2020, with trends from 2010: a systematic analysis. Lancet. 2023;402(10409):1261-1271
18 Perin J, Mulick A, Yeung D, et al. Global, regional, and national causes of under-5 mortality in 2000-19: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet Child Adolesc Health 2022; 6(2): 106-15