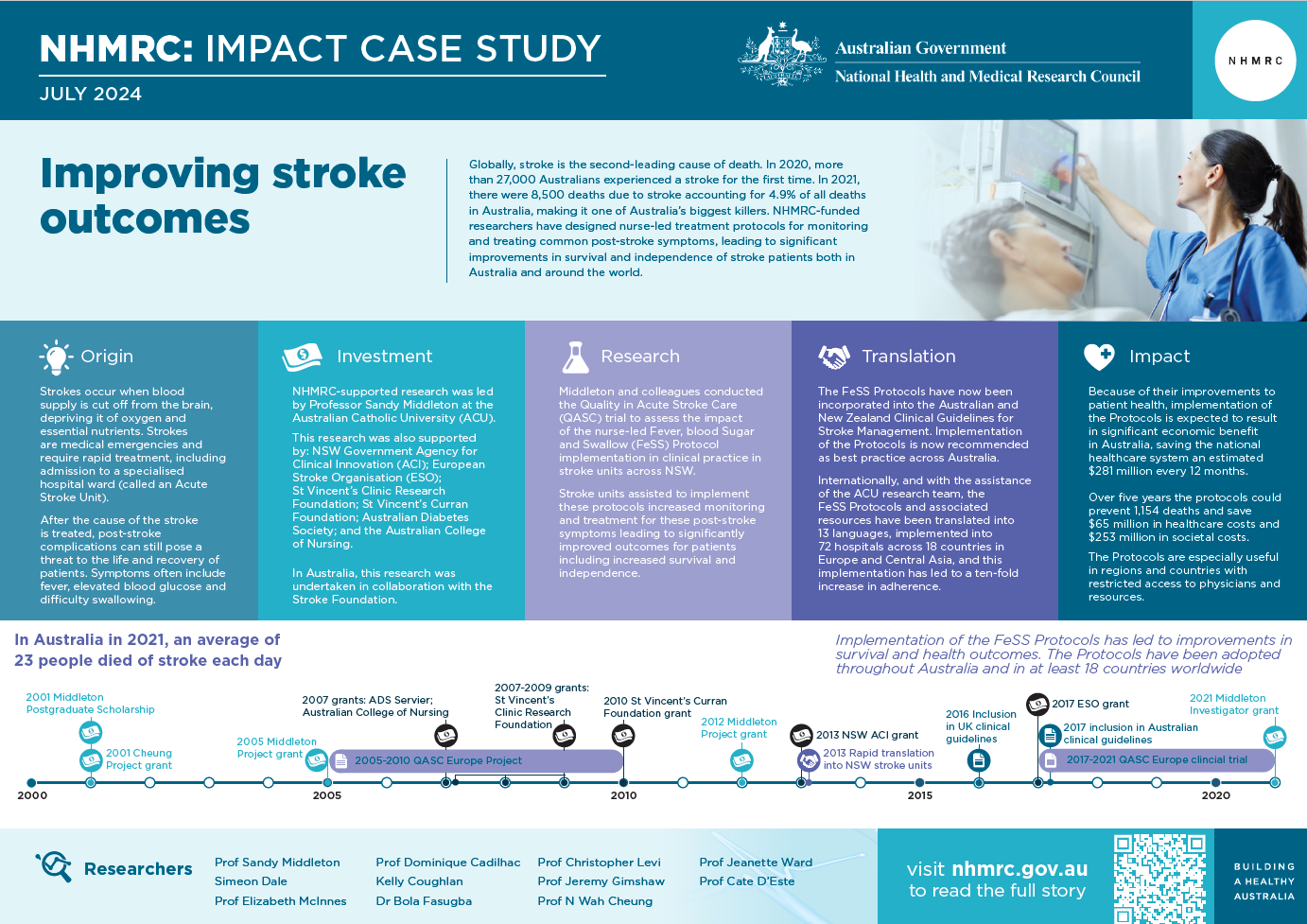
In 2021, an average of 23 people died of stroke each day in Australia, making stroke one of the leading causes of death.1 Acute post-stroke symptoms contribute to this mortality, causing loss of life and independence. A team of NHMRC-funded researchers designed cost-effective and easy to implement protocols for the monitoring and treatment of patients in the 72 hours following a stroke. Implementation of these protocols has led to improvements in survival and health outcomes. They have been adopted into hospitals throughout Australia and in at least 18 countries across the world.
- Video transcript
Professor Sandy Middleton 0.06
Hello. My name is Professor Sandy Middleton. I am the Director of the Nursing Research Institute, which is based at St. Vincent's Hospital in Sydney, and it's a joint collaboration between St. Vincent's Health Network, Sydney and the Australian Catholic University. And I'm also the Professor of Nursing.I'm a nurse trialist, and my area of interest is implementation research. So it's about getting evidence into practice. So it's evidence that we know makes patients better. And I conduct trials around clinician behaviour change and trying to work out the best ways to get that evidence into practice for every single patient.
Simeon Dale 0:46
One set of nurse interventions do have a big effect on patient outcomes after stroke. They're called the FeSS Protocols.Professor Sandy Middleton 0.53
In 2011, our team published a cluster randomized trial of the FeSS Protocols in The Lancet, one of the world's most prestigious medical journals.We tested the effects of the FeSS Protocols in 19 hospitals and 1,600 patients. We randomly assigned some stroke units to receive the FeSS Protocols, alongside some guidance from our team about how to make them part of routine stroke care. The control group only received the existing clinical practice guidelines.
In the Stroke Units who received our support to implement the FeSS Protocols, patients were 16% more likely to be alive and independent 3 months after their stroke.
The FeSS Protocols are 3 nurse led protocols to manage fever, hypoglycaemia or raised glucose levels, and swallowing difficulties after an acute stroke. We know that when we help nurses to implement these protocols, patients are 15% more likely to be alive and independent, 3 months after their stroke and also significantly likely to be alive longer term out to 4 years following their stroke.
But we also know that there are significant financial benefits, and that is $65 million saving in healthcare costs and $251 million saving in societal costs when patients are cared for over a 5 year period using these protocols.
2:21
In 2011, we conducted a cluster randomized control trial where we had 19 acute stroke units in New South Wales, and we assisted 10 of them to implement the FeSS Protocols. And we found that those hospitals where we implemented the protocols, patients were significantly more likely to be alive and independent at 3 months.And then we worked closely with the New South Wales Agency for Clinical Innovation, and we rolled the protocols out across all 36 New South Wales stroke services across the state.
Kirsty Page 2:55
We now have the FeSS Protocols embedded in our stroke care pathway.Professor Sandy Middleton 2.57
The protocols are also spreading across Europe. To successfully implement the FeSS Protocols in 64 hospitals across 17 countries.We're delighted that the FeSS Protocols are now being used overseas in Europe. We have helped work on a study where they have implemented the protocols into 64 hospitals across 17 European countries. Importantly, some of these countries were from Eastern Europe that are not necessarily well resourced and don't always have access to the best stroke therapies, including clot-busting medication.
3.31
So we really feel that our protocols can make a really big difference to patients in these countries. It's really difficult to get evidence into practice. It shouldn't be this hard, but we know that if we just send out protocols like these and ask physical clinicians to start using them, it doesn't happen.So it's really important that we wrapped our FeSS Protocols up in evidence- based implementation science techniques.
Emily (Speech Pathologist/Language Therapist) 3:54
Most patients, it's normal to swallow most medications with water. It's so routine that we don't even think about it. The problem is that for 40% to 80% of patients that have a stroke, their swallowing may be impaired.Professor N Wah Cheung (Endocrinologist) 4:05
It's excellent that many hospitals, like this one assess blood glucose as part of their routine care. For people with stroke, it's so important because hyperglycaemia is very common among stroke patients.Simeon Dale 4:17
With a few evidence-based strategies, many leaders can help their teams to thrive on continual improvement.End of transcript.
Origin
A stroke is a sudden impairment of brain function that occurs when arteries leading to the brain are blocked or ruptured. The resulting lack of blood deprives the brain of vital oxygen and nutrients causing brain cells to die and brain damage to occur.
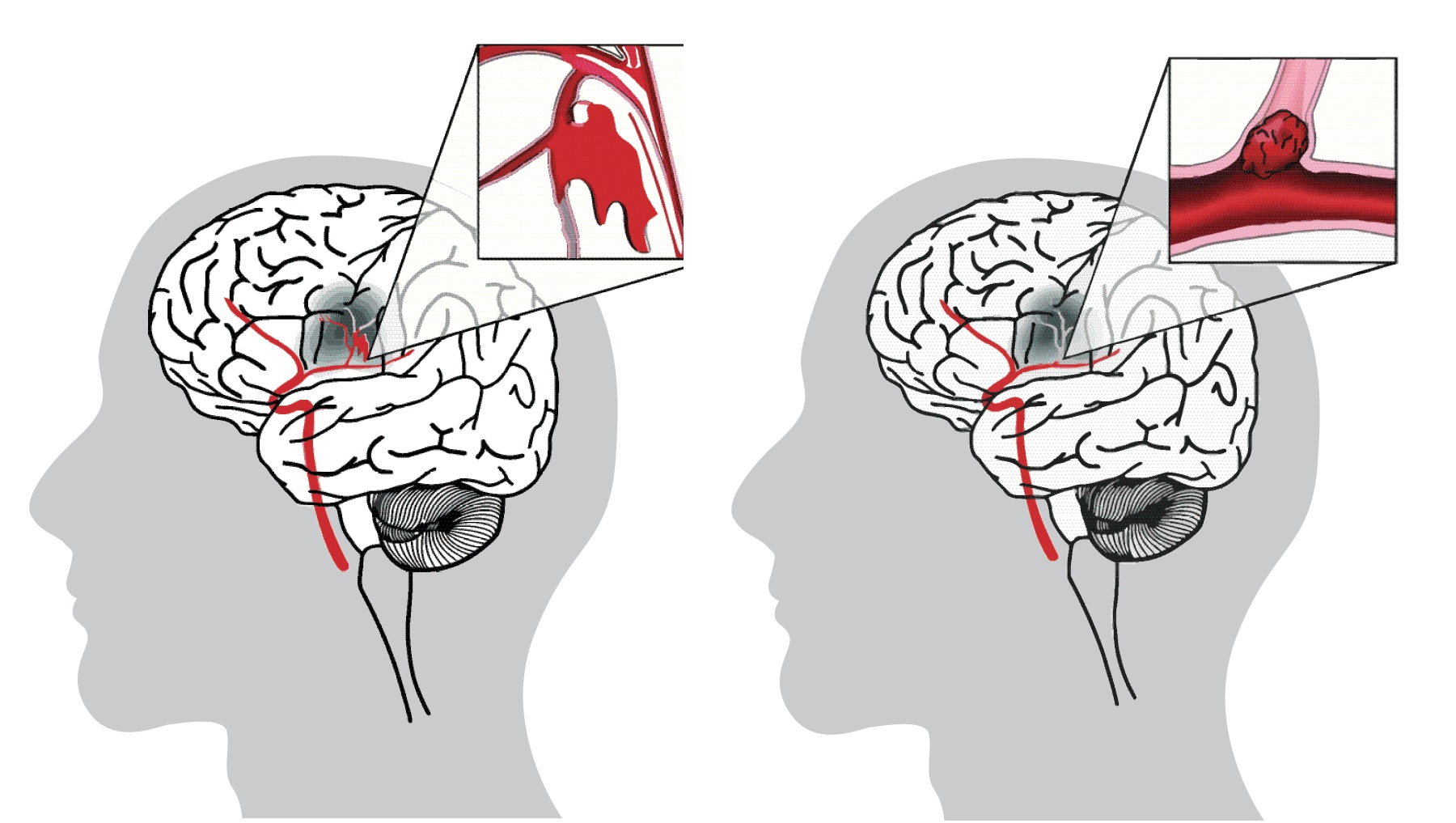
Strokes are medical emergencies and require rapid treatment, including admission to a specialised hospital ward (called an Acute Stroke Unit). Complications in the following 72 hours can still pose a threat to the life and recovery of patients. These often include fever, elevated blood glucose (hyperglycaemia) and difficulty swallowing.
After a stroke, more than 30% of patients develop a fever (body temperature over 37.5°C).2 Prolonged fever in these patients is associated with increased mortality and significantly poorer outcomes.3 Similarly, hyperglycaemia is common after stroke, with 40-60% of stroke patients affected.4 Patients who have hyperglycaemia in the first 48 hours after a stroke have a greater risk of death and disability compared to those with normal blood glucose levels.5
Swallowing difficulty, also called dysphagia, affects about 42% of patients post stroke.6 Dysphagia increases the risk of food or fluid entering the lungs instead of the stomach and can lead to life-threatening chest infections (pneumonia). Early dysphagia screening reduces the risk of pneumonia, mortality, overall dependency and length of stay in hospital.7
During the last quarter of the 20th century, knowledge of these stroke complications and their best treatment options accumulated. 8 One NHMRC-funded research team focused on supporting routine and systematic application of best practices within stroke units globally.
Investment
NHMRC first provided grants for research focused on or relating to stroke in 1942. In 1967, NHMRC encouraged physicians to use and disseminate educational pamphlets related to stroke. These pamphlets included: Up and around from the US Public Health Service; Stroke. The fight back from the National Heart Foundation of Australia; and Stroke Illness from the Chest and Heart Association, London.
Commencing in 2005, research undertaken by Sandy Middleton and her team, based at the Australian Catholic University (ACU) and collaborating institutions, received NHMRC funding to undertake the Quality in Acute Stroke Care (QASC) trial. This team included Christopher Levi, Dominique Cadilhac, Ngai Wah Cheung, Julie Considine, Kelly Coughlan, Simeon Dale, Oyebola Fasugba, Mark Fitzgerald, Richard Gerraty, Rhonda Griffiths, Jeremy Grimshaw, Elizabeth McInnes and Jeanette Ward.
The QASC trial subsequently developed into a program of research funded by further NHMRC grants and received additional grants from the NSW Government Agency for Clinical Innovation (ACI), the European Stroke Organisation (ESO), St Vincent’s Clinic Research Foundation, the St Vincent’s Curran Foundation, the Australian Diabetes Society, and the Australian College of Nursing.
The team also collaborated with:
- (in Australia) the Stroke Foundation and 36 NSW Local Health Districts for the QASC Implementation Project (QASCIP)
- (in Europe) ESO, the Registry of Stroke Care Quality, and the European Acute Networks Striving for Excellence in Stroke (Angels) Initiative.
The PDF poster version of this case study includes a graphical timeline showing NHMRC grants provided and other events described in the case study.
Research
During the early 1980s, when Sandy Middleton was working as a registered nurse in a regular medical ward, there was a lack of proven treatments available for patients who had suffered an acute stroke. The standard care protocol involved a ‘wait-and-see’ approach, as healthcare staff monitored patients for well-known deficits like impaired speech and restricted physical abilities.
However, by late 2003, when she had just finished her PhD examining carotid endarterectomy (a procedure designed to reduce the risk of stroke), the situation had changed considerably. It had recently been shown that stroke unit patients demonstrated improved health outcomes, though it was not known why.9
Middleton discussed this question with Professor Christopher Levi, Director of the stroke unit at the John Hunter Hospital in Newcastle NSW, and Levi suggested it might be associated with fever, blood glucose and swallowing management.
To test this theory, Middleton, Levi and collaborators submitted a successful NHMRC project grant proposal resulting in development, implementation and evaluation of the Fever, Sugar, Swallow (FeSS) Protocols.
The Protocols – which were developed by three expert panels consisting of neurologists, endocrinologists, nurses and speech pathologists, in line with the national stroke and diabetes clinical practice guidelines – are used to guide patient management during the 72 hours following a stroke and involve:
- monitoring patient temperature at least four times a day and promptly treating any elevated temperature (greater than or equal to 37.5°C) with paracetamol
- monitoring patient blood glucose at least four times a day and promptly treating elevated levels (greater than 10mmol/L) with insulin
- ensuring patient screening for dysphagia by a qualified nurse prior to consumption of solids, liquids or medication by mouth, and referring those patients who show signs of dysphagia to a speech pathologist for a full swallowing assessment.
Middleton and colleagues conducted the QASC trial to assess the impact of supported implementation of the nurse-led FeSS Protocols in clinical practice. The QASC trial took place across 19 stroke units in NSW from 2005-2011.
The trial randomised participating stroke units into intervention and control groups. The control stroke units received a summarised copy of existing guidelines. Intervention stroke units, by contrast, received the FeSS Protocols along with training for stroke unit staff in how to implement them and ongoing support provided by site clinical champions and the research team.10
The trial demonstrated that supported implementation of the Protocols had a significant impact on patient health. Three months after their stroke, patients who received treatment in intervention stroke units were 15.7% more likely to be alive and independent than those in the control group. A follow-up study demonstrated that the intervention stroke unit patients had reduced mortality four years after their initial stroke (and were over 20% more likely to be alive).11
Translation
As a consequence of the work of Middleton and colleagues, clinical practice has now changed in Australia and internationally.
During 2012-2014, the team worked with NSW ACI and clinical champions to successfully implement the Protocols within all 36 stroke units/services in NSW.12 Informed by this success, the Protocols have now been incorporated into the Australian and New Zealand Clinical Guidelines for Stroke Management and implementation of the Protocols is now recommended as best practice across Australia.13
An ongoing NHMRC-funded clinical implementation trial is currently underway by the ACU team to assess how best to facilitate the uptake of the Protocols more widely across Australia and New Zealand, including into hospitals in rural and remote areas and in hospitals that may only have a stroke service rather than a dedicated stroke unit.

Internationally, and with the assistance of the ACU research team and the Angels Initiative, the FeSS Protocols (and associated resources) have been translated into 13 languages, implemented into 72 hospitals across 18 countries in Europe and Central Asia, and this implementation has led to a ten-fold increase in FeSS Protocol adherence (from 3.4% to 35%).14
For some of the countries with lower to middle income (e.g. Moldova, Ukraine and Uzbekistan) the Protocols have been particularly important as stroke treatments such as thrombolysis and endovascular clot retrieval have not been routinely available, due to lack of resources. However, implementation of the FeSS Protocols was highly effective in improving stroke management in all countries, irrespective of their income level classification.
More recently, the Protocols have been successfully implemented into eight stroke units in Germany, again demonstrating that implementation of the Protocols is feasible across a range of healthcare systems, independent of the relative income status of the country.15
Outcomes and impacts
Globally, stroke remains the second-leading cause of death.16 In 2020, more than 27,000 Australians experienced a stroke for the first time, adding to the 445,087 stroke survivors living across the country.17 In Australia, every 19 minutes someone will experience a new stroke. In 2021, there were 8,500 deaths due to stroke, accounting for 4.9% of all deaths in Australia.18
However, patients treated in Australian stroke units where the Protocols are being implemented now have a higher likelihood of survival and independence 90 days after their stroke and a higher likelihood of being alive four years after the stroke.
Implementation of the FeSS Protocols is expected to result in significant economic benefit in Australia, saving the national healthcare system an estimated $281 million every 12 months (if intervention is received by only 65% of eligible patients).19 Over five years the protocols could prevent 1,154 deaths and save $65 million in healthcare costs and $253 million in societal costs.20 As total health system expenditure on stroke was estimated to be $1.3 billion in 2020, this represents a significant improvement.21
Importantly, unlike some stroke treatments, the FeSS Protocols are useful for all stroke patients. This, alongside with their economic benefits, nurse-led nature and administrative simplicity, make them especially useful in regions and countries with restricted access to physicians and resources.
From 2011 to 2023, the QASC program of work received 14 awards, acknowledging the extensive contribution this work has made to translational research and impact.
Researchers
Professor Sandy Middleton
Sandy Middleton is a registered nurse and has graduated with a Bachelor of Applied Nursing, a Master of Nursing and a PhD from the University of Sydney. She is currently the Director of Nursing Research Institute at St Vincent’s Health Network Sydney, St Vincent’s Hospital Melbourne and ACU, and has led the QASC program of research. In 2014, the QASC program of work was awarded the NSW Premier's Public Sector Award for Improving Performance and Accountability, and Sandy was awarded the 2014 NSW Health Nursing and Midwifery Award for Excellence in Innovation Research. Sandy is also Director of the Sydney Partnership for Health, Education, Research and Enterprise (SPHERE) Nursing and Midwifery Implementation Science Academy and a Fellow of the Australian Academy of Health and Medical Sciences.
Simeon Dale
Simeon Dale is a Clinical Research Fellow at the Nursing Research Institute. She has 18 years clinical experience in critical care nursing specialising in neuroscience and has practiced nursing in three countries. Simeon is currently working with Sandy on the QASC Australasia Trial. She was the project manager for the QASC Europe project, which supported implementation of the FeSS Protocols into 64 hospitals in 17 countries. She is also working on the Stroke Living Guidelines with the Stroke Foundation and is also the co-chair of Acute Stroke Nurse Education Network.
Professor Elizabeth McInnes
Elizabeth McInnes is currently Deputy Director of the Nursing Research Institute. She has extensive experience in conducting randomised controlled trials (RCTs) and process evaluations focused on improving patient safety using implementation science methods to improve evidence uptake. Her current research focuses on de-implementation of low-value wound care.
Professor Dominique Cadilhac
Dominique Cadilhac has graduated with a Bachelor of Nursing, a Masters of Public Health and a PhD. Her research is focused on improving patient care and outcomes in stroke. She is the Co-Director of Stroke and Ageing Research, School of Clinical Sciences at Monash University and Data Custodian for the Australian Stroke Clinical Registry at the Florey Institute. Her skillset includes epidemiology, implementation research, and economic evaluation.
Kelly Coughlan
Kelly Coughlan comes from a critical care and senior stroke nursing background and has been a clinical research officer at the Nursing Research Institute since 2013. This cross-campus role is specific to stroke and nurse-led research. She has been a working party member of the National Stroke Foundation Clinical and Living Stroke Guidelines since 2015 and is currently enrolled in a PhD program at ACU.
Dr Bola Fasugba
Bola Fasugba is a senior research officer in the Nursing Research Institute. Her background is in medicine and public health research. She is currently managing the QASC Australasia Trial aimed at improving translation of evidence-based nurse-initiated stroke care protocols in hospitals. She has expertise in designing and managing multi-site hospital-based research projects including conducting systematic reviews, RCTs and mixed-methods studies.
Professor Christopher Levi
Christopher Levi is an academic stroke neurologist, Fellow of the Australian Academy of Health and Medical Science, the Executive Director Research and Innovation, Chief Clinical Information Officer and Director of the John Hunter Hospital Health and Innovation Precinct, Hunter New England Local Health District. He is Conjoint Professor of Medicine at The University of Newcastle and between 2017-2021, Professor of Neurology at the University New South Wales and Executive Director of SPHERE, one of Australia's Advanced Health Research and Translation Centres.
Professor Jeremy Grimshaw
Jeremy Grimshaw is an internationally recognized implementation scientist and evidence synthesist. His research focuses on the evaluation of interventions to disseminate and implement evidence-based practice. He is a Senior Scientist, Clinical Epidemiology Program, Ottawa Hospital Research Institute, a Full Professor in the Department of Medicine, University of Ottawa and a Tier 1 Canada Research Chair in Health Knowledge Transfer and Uptake.
Professor Wah Cheung
Ngai Wah Cheung is the Director of Diabetes and Endocrinology at Westmead Hospital. He has served as President of the Australian Diabetes Society, Chair of the National Association of Diabetes Centres, and as a board member of Diabetes Australia. He is currently Co-chair of the Endocrine Network of NSW ACI.
Inpatient diabetes management is one of his key areas of research interest and he is heavily involved in the implementation of evidence-based guidelines and clinical care for people with diabetes.
Professor Jeanette Ward
As one of the earliest champions in Australia for the foundations and applications of evidence-based health care, Jeanette brought her extensive experience as an evidence-user to the design of the first QASC cluster randomised trial (CRT) which commenced in 2005. Jeanette also contributed key methodological advice to the team when conceptualising the T3 CRT. Although her direct connection with this research program reduced upon her relocation to the remote Kimberley, Jeanette has sustained her interest in CRTs including completion of a systematic review about the unique ethical aspects in relation to Aboriginal and Torres Strait Islander peoples. This appeared in the Nulungu Publication Series and has been used by the WA Aboriginal Health Ethics Committee.
Professor Cate D’Este
Catherine D’Este is currently a Senior Advisor at the Sax Institute and Conjoint Professor at The University of Newcastle. Her previous role was Professor of Biostatistics at the Australian National University, and prior to that she was Professor and Chair of Biostatistics at The University of Newcastle. Professor D’Este has approximately 35 years of experience as a biostatistician and has led the design and analysis of a wide array of research projects in population health, covering a variety of study designs and methods such as cross-sectional studies and surveys, cohort studies, audits, analysis of routinely collected administrative health data and disease register data (including linked data), and experimental designs such as individual and cluster RCTs, and stepped-wedge trials.
Partner
This case study was developed with input from Sandy Middleton and Simeon Dale and in partnership with the Australian Catholic University.
References
The information and images from which impact case studies are produced may be obtained from a number of sources including our case study partner, NHMRC’s internal records and publicly available materials. Key sources of information consulted for this case study include:
1 Australian Institute of Health and Welfare. Heart, stroke and vascular disease: Australian facts [Internet]. Canberra: Australian Institute of Health and Welfare, 2023 [cited 2024 Jan. 15]. Available from: https://www.aihw.gov.au/reports/heart-stroke-vascular-disease/hsvd-facts
2 Phipps, MS, Desai, RA, Wira C, & Bravata DM. (2011). Epidemiology and outcomes of fever burden among patients with acute ischemic stroke. Stroke, 42(12), 3357-3362
3 Prasad K, & Krishnan PR. (2010). Fever is associated with doubling of odds of short-term mortality in ischemic stroke: an updated meta-analysis. Acta Neurol Scand, 122(6), 404-408; and Greer, DM, Funk, SE, Reaven, NL, Ouzounelli, M, & Uman, GC. (2008). Impact of fever on outcome in patients with stroke and neurologic injury: a comprehensive meta-analysis. Stroke, 39(11), 3029-3035
4 Gentile NT, Seftchick MW, Huynh T, Kruus LK, Gaughan J. Decreased mortality by normalizing blood glucose after acute ischemic stroke. Academic emergency medicine. 2006 Feb;13(2):174-80; and Saxena A, Anderson CS, Wang X, Sato S, Arima H, Chan E, Muñoz-Venturelli P, Delcourt C, Robinson T, Stapf C, Lavados PM. Prognostic significance of hyperglycemia in acute intracerebral hemorrhage: the INTERACT2 study. Stroke. 2016 Mar;47(3):682-8.
5 Fuentes B, Castillo J, San José B, Leira R, Serena J, Vivancos J, Dávalos A, Nuñez AG, Egido J, Díez-Tejedor E. The prognostic value of capillary glucose levels in acute stroke: the GLycemia in Acute Stroke (GLIAS) study. Stroke. 2009 Feb 1;40(2):562-8; and Capes SE, Hunt D, Malmberg K, Pathak P & Gerstein HC. (2001). Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke, 32(10), 2426-2432
6 Sherman V, Greco E & Martino R. (2021). The Benefit of Dysphagia Screening in Adult Patients with Stroke: A Meta-Analysis. J Am Heart Assoc, 10(12), e018753
7 Bray, BD, Smith, CJ, Cloud, GC, Enderby, P, James, M., Paley, L, ... & Rudd, AG. (2017). The association between delays in screening for and assessing dysphagia after acute stroke, and the risk of stroke-associated pneumonia. Journal of Neurology, Neurosurgery & Psychiatry, 88(1), 25-30; and Banda, KJ, Chu, H, Kang, XL. et al. Prevalence of dysphagia and risk of pneumonia and mortality in acute stroke patients: a meta-analysis. BMC Geriatr22, 420 (2022)
8 Melamed E. Reactive hyperglycaemia in patients with acute stroke. Journal of the neurological sciences. 1976 Oct 1;29(2-4):267-75; and DePippo KL, Holas MA, Reding MJ. Validation of the 3-oz water swallow test for aspiration following stroke. Archives of neurology. 1992 Dec 1;49(12):1259-61; and Greer DM, Funk SE, Reaven NL, Ouzounelli M, Uman GC. Impact of fever on outcome in patients with stroke and neurologic injury: a comprehensive meta-analysis. Stroke. 2008 Nov 1;39(11):3029-35
9 Langhorne P, Duncan P. Does the organization of postacute stroke care really matter? Stroke. 2001 Jan;32(1):268-74
10 Middleton S, McElduff P, Ward J, Grimshaw JM, Dale S, D'Este C, Drury P, Griffiths R, Cheung NW, Quinn C, Evans M. Implementation of evidence-based treatment protocols to manage fever, hyperglycaemia, and swallowing dysfunction in acute stroke (QASC): a cluster randomised controlled trial. The Lancet. 2011 Nov 12;378(9804):1699-706
11 Middleton S, Coughlan K, Mnatzaganian G, Low Choy N, Dale S, Jammali-Blasi A, Levi C, Grimshaw JM, Ward J, Cadilhac DA, McElduff P. Mortality reduction for fever, hyperglycemia, and swallowing nurse-initiated stroke intervention: QASC trial (Quality in Acute Stroke Care) follow-up. Stroke. 2017 May;48(5):1331-6
12 Middleton S, Lydtin A, Comerford D, Cadilhac DA, McElduff P, Dale S, et al. From QASC to QASCIP: successful Australian translational scale-up and spread of a proven intervention in acute stroke using a prospective pre-test/post-test study design. BMJ Open. 2016;6(5).
13 Stroke Foundation. Clinical Guidelines for Stroke Management. Available at https://informme.org.au/guidelines/living-clinical-guidelines-for-stroke-management. Accessed 15 January 2024
14 Middleton S, Dale S, McElduff B, Coughlan K, McInnes E, Mikulik R, Fischer T, Van der Merwe J, Cadilhac D, D’Este C, Levi C. Translation of nurse-initiated protocols to manage fever, hyperglycaemia and swallowing following stroke across Europe (QASC Europe): A pre-test/post-test implementation study. European Stroke Journal. 2023 Mar;8(1):132-47
15 Cassier-Woidasky A, Middleton S, Dale S, McElduff B, Coughlan K, McInnes E, Cadilhac D, & Pfeilschifter W. Quality in Acute Stroke Care (QASC) Germany Project: Improving efficiency in Stroke Units with nurse-initiated protocols to manage Fever, Hyperglycaemia and Swallowing post stroke. European Stroke Journal 2023; 8(2_suppl): 3-669. [Oral presentation European Stroke Conference 2023 Munich, Germany]
16 Feigin VL, Stark BA, Johnson CO, Roth GA, Bisignano C, Abady GG, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet Neurology. 2021;20(10):795-820
17 Stroke Foundation. 2020. No Postcode Untouched: Stroke in Australia 2020. Sydney: Deloitte Access Economics
18 Australian Institute of Health and Welfare. Heart, stroke and vascular disease: Australian facts [Internet]. Canberra: Australian Institute of Health and Welfare, 2023 [cited 2024 Jan. 15]. Available from: https://www.aihw.gov.au/reports/heart-stroke-vascular-disease/hsvd-facts
19Australian Clinical Trials Alliance. (2017). Economic evaluation of investigator-initiated clinical trials conducted by networks. Sydney: ACSHQC
20 Marquina C, Ademi Z, Zomer E, et al. Cost Burden and Cost-Effective Analysis of the Nationwide Implementation of the Quality in Acute Stroke Care Protocol in Australia. Journal of Stroke and Cerebrovascular Diseases 2021; 30
21 Deloitte Access Economics DA. The economic impact of stroke in Australia 2020. Stroke Foundation, November 2020.

