For the review of the evidence for dietary guidance for older Australians.
Published in June 2024.
Publication Data
Table of contents
Background
In late-2023 the Department of Health and Aged Care requested that the NHMRC provide advice for older Australians to support health and wellbeing as an additional component of the revision of the Australian Dietary Guidelines. This guidance will cover the general population aged 65 years and older (or 50+ years for Aboriginal and Torres Strait Islander peoples). The guidance will not apply to people with medical conditions that require specialised diets for managing disease or frailty. However, it is aimed at supporting prevention of malnutrition, frailty, falls and chronic conditions.
Purpose
This document describes the process the Dietary Guidelines Expert Committee (the Expert Committee) used to shortlist topics and research questions for older Australians to target the scope of the evidence review within the available resources.
The Prioritisation Process Report for the review of the evidence underpinning the broader Australian Dietary Guidelines can be found on the NHMRC website. This information also helped inform the prioritisation work undertaken for the Guidelines for Older Australians. The Prioritisation Process Report for Older Australians includes:
Section 1 – Scoping activities – describes activities which contributed to Expert Committee consideration of a broad list of topic areas relevant to nutrition and food-based advice for older Australians.
Section 2 – Topic prioritisation – this is similar to the Expert Committee process to reach a refined list of topic areas for the broader guideline revision (more information can be found in can be found in the Prioritisation Process Report).
Section 3 – Next steps for developing dietary guidance for older Australians
- Research question development and prioritisation - describes the process to develop a broad list of in-scope research questions and identify their relative priority.
- Guidance on the review process including the literature search for systematic reviews of priority topics and public call for systematic reviews.
1. Scoping activities
During 2020 and 2021, NHMRC carried out scoping activities for the revision of the broader Australian Dietary Guidelines. Scoping activities were intentionally broad, involving web searches, literature database searches and media platform searches. Direct input was sought from stakeholders through surveys and targeted consultation on various aspects of the 2013 Guidelines and companion resources, such as the Australian Guide to Healthy Eating and the Aboriginal and Torres Strait Islander Guide to Healthy Eating.
Dietary guidance for older Australians scoping
Specific scoping activities undertaken for the older Australians review included:
- Health and nutrition of older Australians - environment scan, (Attachment A). A high-level summary of the health and nutrition status of older Australians, outcomes of interest and key Australian Government policy. This includes a summary of possible outcomes of poor nutrition in older adults as well as an overview of the current relevant Australian policy. Completed October 2023.
- Summary of international guidelines for older people, (Attachment B). A summary of international dietary guidelines for older people considered to be relevant to Australia. Four guidelines from Finland, Ireland, the United Kingdom, and the United States of America were identified. Completed October 2023.
- Stakeholder scoping survey – themes related to older Australians (Attachment C). In 2021, during initial scoping activities for the revision of the Australian Dietary Guidelines, NHMRC conducted an anonymous online survey of stakeholders (see the broader prioritisation report). Additional analyses of the stakeholder scoping survey raw data were undertaken in October 2023 to identify themes related to healthy ageing and/or dietary guidelines for older Australians.
- Ageing targeted consultation summary (Attachment D). A summary of key themes identified during targeted consultation with organisations and individuals who work with older Australians. Consultations were held in October and November 2023.
2. Topic prioritisation
The Expert Committee had previously identified priority research topics and healthy ageing specific outcomes during the prioritisation process for the broader Australian Dietary Guidelines. To do so, Expert Committee members participated in a series of surveys and discussions to agree on a shortlist of topic areas using the principles outlined below.
Prioritisation for older Australians followed the same principles for prioritising topics as the previous work that was done for the broader Australian Dietary Guidelines. This process occurred in April 2024.
Principles for topic prioritisation
The following principles were applied by the Expert Committee when prioritising the topics for the broader Australian Dietary Guidelines and when considering the shortlisted topics during topic prioritisation for older Australians:
- Relevance
- Importance
- Type of impact
- Degree of impact.
The principles were modelled on the prioritisation pathways used for development of the Dietary Guidelines for Americans 2021–25, the Nordic Nutrition Recommendations 2022, and Canada’s Dietary Guidelines. The principles also took into consideration prioritisation criteria commonly used in the development of health practice guidelines.1
More information on the prioritisation principles can be found in Prioritisation Process Report for the review of the broader Australian Dietary Guidelines.
Summary of shortlisted topics
The list of potential topic areas was developed using results from the scoping activities (see Section 1). The following broad topics were shortlisted to inform development of the research questions and scope of the evidence review update:2
- Adequate protein intake
- Adequate fluid intake
- Sodium
- Limit saturated fat
- Maintain dietary fibre
- Physical activity
- Energy recommendations
- Effect of medicines on nutrition
- Food safety
- Alcohol
- Carbohydrate/sugar
- Dairy/calcium
- Plant based diets
- Micronutrient requirements – for example, vitamin B, vitamin D and zinc
- Food security
- Nutrition of maintenance for weight and muscle mass
- Anti-inflammatory diets
- Supplements.
Prioritisation of topics
The Expert Committee considered the potential topics for older Australians using the prioritisation principles. Many topics were considered to be covered by the research questions already identified during prioritisation for the broader Australian Dietary Guidelines revision (Tables 1–5). Others were identified as being able to be addressed by alternative avenues (for example sodium, alcohol; Table 6). Some were out of scope as they were not related to whole foods or dietary patterns or were considered to be implementation issues (Tables 7–8).
The Expert Committee advised the previously identified Dietary Guidelines review questions were relevant to, and are a priority for, older Australians. The Expert Committee advised that no new topics were required.
Expert Committee members advised that contextual factors that affect older Australians, and are barriers to consuming a diet aligned with the guidelines, may be different from those that affect the general population. Contextual factors considered of particular relevance include:
- changes in taste and smell
- oral health
- decline in appetite
- eating alone
- mobility/dexterity
- activities of daily living.
In addition, provision of food by residential aged care facilities may be a barrier to consuming a diet aligned with the guidelines.
Updates to outcomes
As part of the broader Dietary Guidelines revision, the Expert Committee identified the following outcomes as being of interest:
- All cause mortality
- All cause morbidity
- Cancer risk factors
- Cardiovascular disease risk or related factors
- Type 2 diabetes risk or related factors
- Overweight/obesity or related size measures
- Mental health (depression and anxiety)
- Gastrointestinal health
- Quality of life
- Neurocognitive health including dementia
- Sarcopenia
- Bone health.
Following the scoping for older Australians the Expert Committee advised that outcomes specifically relevant to older Australians should be added:
- Falls
- Frailty
- Malnutrition
- Fracture
- Healthy weight range for older adults.
| Question/subtopic | Populations | Interventions/ exposures, comparisons | Outcomes | Notes |
|---|---|---|---|---|
Dietary patterns and health outcomes Dietary patterns must be relevant at a population level. Excludes interventions/ exposures that are for treatment of disease e.g., diabetes, CVD | Older Australians Defined as adults 65+ years or Aboriginal and Torres Strait Islander people aged 50+ | Dietary patterns vs other dietary patterns OR High similarity to a specific dietary pattern vs low similarity to that dietary pattern | Relevant health outcomes
Chronic condition risk factors
Healthy Ageing
| Considered to cover the following topics identified in scoping activities:
|
Intake of animal vs plant sources of protein and health outcomes Excludes interventions/ exposures that are for treatment of disease e.g., diabetes, CVD | Older Australians Defined as adults 65+ years or Aboriginal and Torres Strait Islander people aged 50+ | Protein intake from plant-based sources vs protein intake from animal sources high vs low intake of plant foods | Relevant health outcomes
Chronic condition risk factors
Healthy Ageing
| Considered to cover the following topics identified in scoping activities:
|
| Question/subtopic | Populations | Interventions/ exposures, comparisons | Outcomes | Notes |
|---|---|---|---|---|
Ultra-processed food intake and health outcomes Exclude interventions/ exposures that are for treatment of disease e.g., diabetes, CVD | Older Australians Defined as adults 65+ years or Aboriginal and Torres Strait Islander people aged 50+ | High intake of ultra-processed foods vs no/low intake of ultra-processed foods | Relevant health outcomes
Chronic condition risk factors
Healthy Ageing
| Considered to cover the following topics identified in scoping activities:
|
| Question/subtopic | Populations | Interventions/ exposures, comparisons | Outcomes | Notes |
|---|---|---|---|---|
Frequency of eating and health outcomes Exclude interventions/ exposures that are for treatment of disease e.g., diabetes, CVD | Older Australians Defined as adults 65+ years or Aboriginal and Torres Strait Islander people aged 50+ | Frequency of eating vs Different meal pattern frequency OR varying levels of frequency of eating OR different meals patterns | Relevant health outcomes
Chronic condition risk factors
Healthy Ageing
| Considered to supplement the dietary patterns question above and cover the following topics identified in scoping activities:
|
| Question/subtopic | Populations | Interventions/ exposures, comparisons | Outcomes | Notes |
|---|---|---|---|---|
Meats, poultry, fish, eggs, nuts and seeds, legumes/beans (including pulses and tofu) Exclude interventions/ exposures that are for treatment of disease e.g., diabetes, CVD | Older Australians Defined as adults 65+ years or Aboriginal and Torres Strait Islander people aged 50+ | Red meat intake vs white meat OR High intake of legumes/ pulses vs No/ low intake of legumes/ pulses | Relevant health outcomes
Chronic condition risk factors
Healthy Ageing
| Considered to supplement the dietary patterns question above and cover the following topics identified in scoping activities:
|
| Question/subtopic | Populations | Interventions/ exposures, comparisons | Outcomes |
|---|---|---|---|
| Influence of eating environment/ context and consumption aligned with guidelines | Older Adults Defined as adults 65+ years or Aboriginal and Torres Strait Islander people aged 50+ Subpopulations of interest: Priority populations identified in the National Preventive Health Strategy 2021 -2030:
| Factors relating to eating environment/ context, including:
Exclude interventions/ exposures that are for treatment of disease e.g., diabetes, CVD | Consumption aligned with guidelines (at point in time; life course) |
| Barriers and enablers to consumption aligned with guidelines | Older Adults Defined as adults 65+ years or Aboriginal and Torres Strait Islander people aged 50+ Subpopulations of interest: Priority populations identified in the National Preventive Health Strategy 2021 -2030:
| Other barriers and enablers to consumption of foods aligned with guidelines e.g., food literacy/skills
Exclude interventions/ exposures that are for treatment of disease e.g., diabetes, CVD | Consumption aligned with guidelines (at point in time; life course) |
| Barriers and enablers to consumption aligned with guidelines | Older Adults Defined as adults 65+ years or Aboriginal and Torres Strait Islander people aged 50+ Subpopulations of interest: Priority populations identified in the National Preventive Health Strategy 2021 -2030:
| Food security Exclude interventions/ exposures that are for treatment of disease e.g., diabetes, CVD | Consumption aligned with guidelines (at point in time; life course) |
| Interventions /strategies to improve dietary patterns and eating behaviours aligned with the guidelines across the life course | Older Adults Defined as adults 65+ years or Aboriginal and Torres Strait Islander people aged 50+ Subpopulations of interest: Priority populations identified in the National Preventive Health Strategy 2021 -2030:
| Interventions Exclude interventions/ exposures that are for treatment of disease e.g., diabetes, CVD | Consumption aligned with guidelines (at point in time; life course) |
| Question/ Subtopic | Rationale for priority |
|---|---|
| Sodium / salt intake and health outcomes | Sodium/salt intake and health outcomes to be addressed based on existing NHMRC evidence reviews / recommendations (NRVs 2017 and current update) |
| Alcohol intake and health outcomes | Alcohol intake and health outcomes to be addressed based on existing NHMRC evidence reviews / recommendations (NHMRC Alcohol Guidelines 2020) |
| Food safety outcomes | Food safety aspects to be addressed based on existing National food safety advice, e.g., Food Safety Information Council |
| Physical activity levels | Physical activity aspects to be addressed based on National Physical Activity Guidelines |
| Adequate fluid intake | Considered during evidence to decision process |
| Question/ Subtopic | Rationale for priority |
|---|---|
| Effects of medicines on nutrition | Not related to whole foods, food groups or dietary patterns |
| Micronutrients (vitamin B, vitamin D, zinc, etc) | Not related to whole foods, food groups or dietary patterns |
| Supplements | Not related to whole foods, food groups or dietary patterns |
| Question/ Subtopic | Rationale for priority |
|---|---|
| Guidelines as stand alone | Implementation |
| Specific resource for older Australians | Implementation |
3. Next steps for the dietary guidance for older Australians
To make efficient use of the limited review resources, recent, high quality published systematic reviews addressing the priority research questions will be used where available. A limited number of new evidence reviews will be commissioned, to target key gaps identified in the evidence base. To facilitate this approach, the next phase of the review for older Australians will comprise:
- additional scoping to identify suitable systematic reviews in the recent published literature
- evidence mapping to identify which priority research questions may be answered using existing systematic reviews and to identify gaps in the systematic review literature
- selection of existing systematic reviews and research questions for newly commissioned evidence reviews.
Review identification
Potentially relevant systematic reviews will be identified and sourced via:
- Literature searches, including database searching and searches of systematic reviews commissioned or conducted by key international groups3
- A public call for systematic reviews.
This process aims to identify suitable (current, comprehensive and methodologically robust) systematic reviews for each priority research question.4 It does not aim, or purport, to comprehensively search for and identify every relevant systematic review for the broad priority research questions identified.
Please see the Prioritisation Process Report for the broader Australian Dietary Guidelines for details on how lower priority research questions will be addressed.
Evidence mapping
Systematic reviews identified through the literature searches and public call will be collated and screened against eligibility criteria (including minimum methodological criteria). The risk of bias of potentially eligible reviews will then be assessed.
Eligible systematic reviews will be mapped against the research questions to allow the Expert Committee to consider options for addressing each priority research question and identify gaps in the underlying evidence base, that may be targeted by a newly commissioned evidence review.
Very high or high priority research questions that are unable to be addressed within the available resources will be noted as evidence gaps to inform future reviews.5
Figure 1 provides an overview of the next steps for how information from the literature search and public call will be considered.
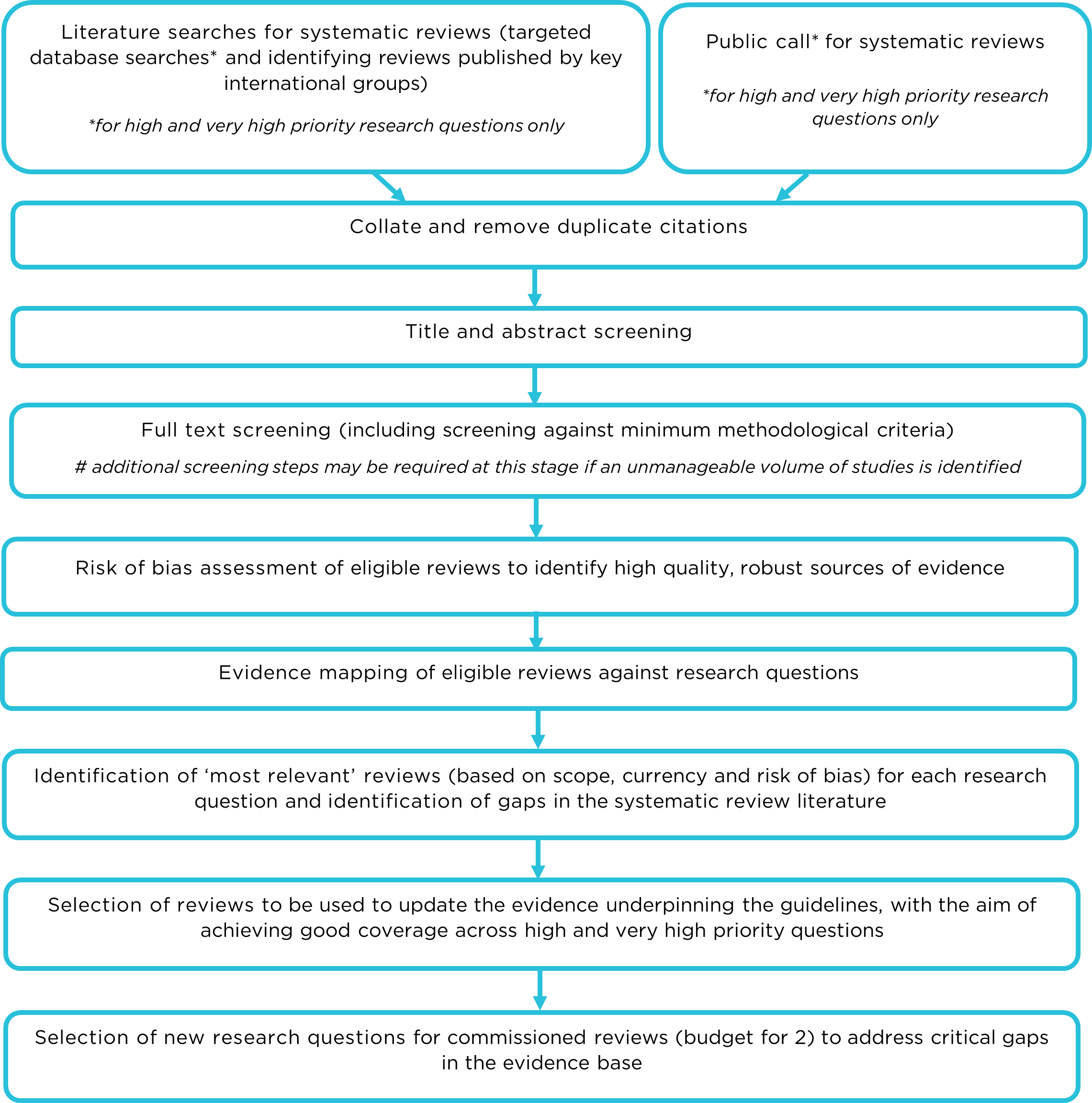
Description of Figure 1 - Overview of scoping and evidence mapping process:
- The process begins with literature searches for systematic reviews (targeted database searches* and identifying reviews published by key international groups) or a Public call* for systematic reviews.
- Collate and remove duplicate citations
- Title and abstract screening
- Full text screening (including screening against minimum methodological criteria) Additional screening steps may be required at this stage if an unmanageable volume of studies is identified
- Risk of bias assessment of eligible reviews to identify high quality, robust sources of evidence
- Evidence mapping of eligible reviews against research questions
- Identification of ‘most relevant’ reviews (based on scope, currency and risk of bias) for each research question and identification of gaps in the systematic review literature
- Selection of reviews to be used to update the evidence underpinning the guidelines, with the aim of achieving good coverage across high and very high priority questions
- Selection of new research questions for commissioned reviews (budget for 2) to address critical gaps in the evidence base
*for high and very high priority research questions only
Endnotes
1 El-Harakeh, A., Morsi, R.Z., Fadlallah, R., Bou-Karroum, L., Lotfi, T., Akl, E.A., 2019. ‘Prioritization approaches in the development of health practice guidelines: a systematic review’, BMC Health Services Research, 19: 692.
2 The list was ranked using prioritisation principles and considering whether the evidence for a topic was likely to have changed significantly since the 2013 guidelines.
3 ‘Key international groups’ with robust methodological processes similar to NHMRC standards (https://www.nhmrc.gov.au/guidelinesforguidelines/standards) identified based on the process adopted by the 2022 Nordic Nutrition Recommendations Group
4 The Expert Committee noted a five-year cut off is common when searching for systematic reviews, the reviews themselves may include primary studies published prior to this. In addition, the revised Guidelines are anticipated for release in 2026 and any systematic review completed prior to 2018 would not consider subsequent recent studies.
5 Funding for the review allows the commissioning of up to 5 de novo reviews, depending on cost and scope.


